Depression and Neurotransmitters
Depression is a serious psychiatric condition that affects many people. It involves the mood, mind and body of patients, who feel hopeless and experience a sense of hopelessness, uselessness and helplessness.
.jpg)
Monoamines are synthesized within the presynaptic nerve termination, stored in vesicles and then released in the synaptic wall (the space between the presynaptic and postsynaptic nerve terminals) in response to certain stimuli.
Once released from the deposits, the monoamines interact with their own receptors - both presynaptic and postsynaptic - in order to carry out their biological activity.
In this way the transmission of the nerve impulse from one neuron to the other is made possible.
After carrying out their function, the monoamines bind to the receptors responsible for their reuptake (SERT for the reuptake of serotonin and NET for the reuptake of norepinephrine) and return inside the presynaptic nerve terminal.
Serotonin (5-HT) is considered the major neurotransmitter involved in depressive pathologies and alterations in its concentration have been associated with many mood disorders.
The selective serotonin reuptake inhibitors (or SSRIs) are able - as the name implies - to inhibit the reuptake of serotonin inside the presynaptic termination, favoring the increase of the 5-HT signal. This increase leads to an improvement in the depressive pathology.
History
The first antidepressants to be synthesized were TCAs (tricyclic antidepressants). However, it was noted that these antidepressants - in addition to inhibiting monoamine reuptake - also blocked other systems in the body, causing a long list of side effects, some of them very serious.
Since already with the use of the first antidepressants it was evident that serotonin had a role in the etiology of depression, the aim of pharmaceutical chemists was to identify and synthesize the ideal SSRI, with the aim of obtaining a highly selective drug for the transporter of serotonin reuptake and that it had little - or no - affinity towards the neuroreceptors responsible for the side effects of TCAs.
_2.jpg)
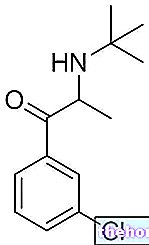
Zimeldina - Chemical Structure
The first success was achieved with the synthesis of zimeldine, a derivative of the tricyclic antidepressant amitriptyline. This molecule, in fact, was able to selectively inhibit the reuptake of 5-HT, with a minimal effect on the reuptake of norepinephrine; more importantly, zimeldine did not have the typical side effects of the TCAs.
Zimeldine thus became the model for the development of future SSRIs.
Classification
SSRIs can be classified based on their chemical structure as follows:
- Phenoxy phenylalkylamines, such as fluoxetine, paroxetine, citalopram and escitalopram;
- Phenylalkylamines, such as sertraline;
- Other types of SSRIs (such as, for example, fluvoxamine).
Mechanism of action
SSRIs inhibit the transporter responsible for serotonin reuptake (SERT) and have little or no affinity for norepinephrine reuptake transport.
Due to their high affinity for SERT, SSRIs inhibit the binding of serotonin to its transporter. This inhibition results in a longer stay of 5-HT in the synaptic wall. In this way, serotonin is able to interact with its receptors - both presynaptic and postsynaptic - for a longer time. This greater receptor interaction leads to an increase in serotonergic transmission.
Furthermore, it appears that prolonged treatment with SSRIs leads to a reduction in the binding sites for serotonin on the SERT, thus causing a reduction in the functionality of the transporter itself which is no longer able to bind - hence re-uptake - large amounts of 5- HT.
_3.jpg)




















-nelle-carni-di-maiale.jpg)




