Generally, this investigation is an integral part of the colposcopy, with which it shares the indications, but it can also be performed alone.
Vulvoscopy can be useful to highlight inflammation, ongoing infections or degenerative processes affecting the external female genitalia. The examination also allows to diagnose preneoplastic and tumor lesions of the vulva.
and a portion of the cervix.Vulva: what it is and where it is
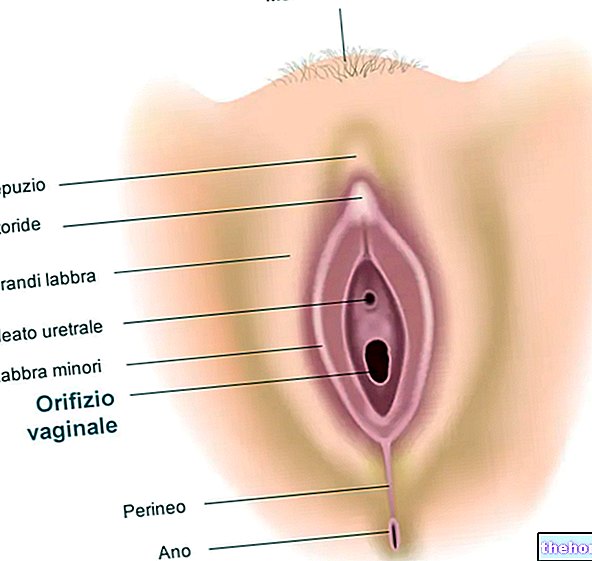
The vulva is the region surrounding the access to the vagina, formed by the clitoris, large and small labia, hymen, external orifice of the urethra, Bartholin's glands and vaginal vestibule.
(or Monte di Venere): relief of skin and underlying adipose tissue centrally located in the pelvic region;
In the vulvar complex there are also the hymen, the external orifice of the urethra (or urinary meatus) and the outlet of the vaginal glands.
Vulvoscopy also allows the examination of the perineum, ie the rhomboid-shaped area that extends sagittally from the lower margin of the pubic symphysis to the apex of the coccyx. Transversely, the perineal region is included between an ischial tuberosity of the " iliac bone and the other.
Vulvoscopy: why is it done?
Vulvoscopy is a "second level gynecological diagnostic investigation. This examination" confirms or excludes the presence of vulvar diseases and helps to establish an adequate therapeutic procedure even in the infectious, inflammatory, neoplastic or degenerative vulvar forms of difficult pathological classification.
The main indications for the execution of the vulvoscopic examination are:
- Presence of persistent symptoms and / or resistant to the most common treatments, such as vulvar itching and / or burning;
- Clinical finding of lesions, ulcers, growths or pigmented areas on the vulva or perineum;
- Early diagnosis of preneoplastic and neoplastic pathology of the vulva.
The lesions that can be highlighted with vulvoscopy are numerous: infectious, inflammatory, skin degenerative, etc. As for colposcopy, also for these vulvar alterations they are defined with a specific terminology: for example, the acronym VIN (acronym of "Vulvar Intraepithelial Neoplasia") is indicative of a vulvar intraepithelial neoplasia and corresponds to the" equivalent CIN at the cervical level. "
Vulvoscopy: when is it indicated?
The execution of vulvoscopy is indicated to diagnose and monitor the evolution of pathological conditions affecting the vulva, such as:
- Chronic vulvar itching;
- Vulvitis (or vulvovaginitis);
- Human papilloma virus (HPV) infection;
- Vulvar lichen sclerosus;
- Vulvar lichen planus;
- Vulvar psoriasis;
- Vulvar skin degenerations characteristic of old age;
- Genital herpes and other sexually transmitted diseases (chlamydia, gonorrhea, etc.);
- Vulvar intraepithelial neoplasia (VIN);
- Cancer of the vulva (quite rare).
Complementary examinations to Vulvoscopy
Normally, vulvoscopic examination is indicated as a complementary investigation to the Pap test and colposcopy.
Depending on the diagnostic suspicion, to understand the nature of a specific problem, the doctor may subject the patient to other tests aimed at deepening the clinical picture, including:
- Biopsy in the presence of a suspicious lesion;
- Microbiological tests with culture methods or molecular analyzes, such as the polymerase chain reaction (PCR), to search for microorganisms responsible for sexually transmitted diseases (eg. Neisseria gonorrhoeae, Chlamydia trachomatis etc.);
- Microscopic examination of vaginal secretions to identify genital infections (e.g. trichomoniasis, bacterial vulvovaginitis, candidiasis, etc.).
The gynecologist performs vulvoscopy focusing on the hymen, clitoris, large and small labia, urinary meatus, outlet of the vaginal glands and perineum.
With the instrumental apparatus (colposcope), the possible presence of:
- Signs of infection;
- Malformations;
- Inflammation or other abnormalities, such as:
- Swellings
- Erythema;
- Changes in pigmentation;
- Hematomas;
- Ulcerations;
- Nodules.
The vulvoscopic examination of the large and small lips allows to highlight painful points, redness, swelling or abnormal secretions. During vulvoscopy, moreover, signs indicative of genital herpes (groups of small vesicles), lichen simplex (evocative external traumas, such as scratching, for a vulvar itch), condyloma acuminata (growths at the perianal or vulvar level) and bartholinitis (inflammation of the Bartholin's glands). The alterations of the regional lymph nodes may be related, however, to sexually transmitted diseases or neoplastic processes.
The observation is followed by palpation of the vulvar region and the eventual execution of a targeted biopsy which can be performed, after local anesthesia, with special punches, diathermic snaps or scalpels.
Vulvoscopy: by whom is it performed?
Vulvoscopy is performed by a gynecologist, a physician who specializes in the physiology and pathology of the female genital system.
How long does the exam last?
Normally, it takes about 30 minutes to perform vulvoscopy.
, local medications (vaginal pessaries or creams) or tampons.In order not to invalidate or influence the outcome of the vulvoscopic examination, the patient is also recommended to:
- Refrain from sexual intercourse 48 hours before the exam;
- Do not shave the intimate region 48 hours before the exam.
For a correct interpretation of the results, on the day of the examination it is advisable to bring with you the results of the last Pap test, in addition to the reports of previous colposcopies, vulvoscopies and biopsies.
.
In order to reduce risks and complications, it is necessary to communicate to the gynecologist who performs the vulvoscopy the possible state of pregnancy, the intake of any drugs (especially antiplatelet and anticoagulants) and the presence of allergies or heart disease (eg mitral prolapse) ).
Vulvoscopy: can it be done with menstruation?
Another indication is to "avoid undergoing vulvoscopy during the period in which menstrual flow is present. Vaginal bleeding could hinder, in fact, the interpretation of the examination. The best period to perform vulvoscopy is from 10 to 18 degrees. day from the beginning of the menstrual cycle.
In the event that the onset of the flow unexpectedly arrives a few days before the vulvoscopy, it is advisable to evaluate with your gynecologist whether it is appropriate to postpone the appointment to a "different date", with the exception of urgent situations.