Generality
Gastroscopy is a diagnostic test that allows the visual exploration of the upper digestive tract (esophagus, stomach and duodenum), in order to exclude or highlight suspected functional alterations or diseases; for this reason, we speak more correctly of esophagus-gastroduodenoscopy (EGDs) .

In recent years, the traditional gastroscopic technique has been flanked by the so-called "trans-nasal gastroscopy", in which access to the upper tracts of the digestive system is via an even thinner endoscope introduced through the nose.
Indications
Why is it done?
Gastroscopy is performed when there is a suspicion of a pathology in the esophagus, stomach or duodenum, for example to investigate some symptoms, such as bleeding (hematemesis = emission of blood from the mouth, melaena = emission of dark and tarry stools) , anemic pictures, pain, retrosternal burning, nausea and difficulty in swallowing (dysphagia).
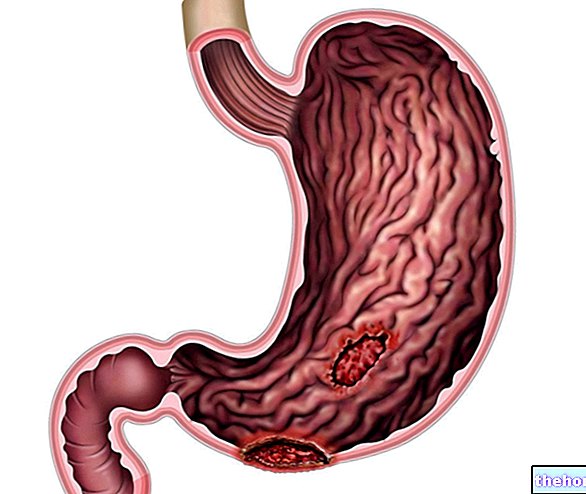
Among the main and most common lesions encountered during a gastroscopy, we remember: esophagitis, Barrett's esophagus, complications related to liver cirrhosis and portal hypertension (esophageal varices), esophageal neoplasms, gastritis, gastric ulcer, gastric neoplasms and duodenal ulcer .
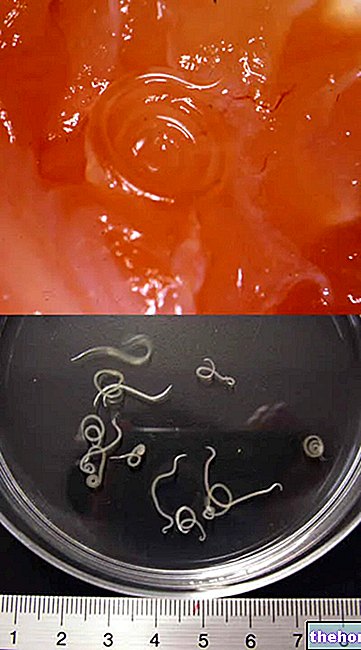
At other times, gastroscopy is performed to monitor the evolution of an already diagnosed disease, the therapeutic efficacy or to perform endoscopic treatments; for example, the doctor can stretch areas affected by stenosis (esophageal narrowing), remove polyps (generally benign growths) or foreign bodies accidentally ingested, stop bleeding, inject drugs or place therapeutic aids, without forgetting the possibility of collecting tissue samples (biopsy ) to search for infections (Helicobacter pylori), for the verification of the good functioning of the intestine and for the diagnosis of abnormal-looking tissues, which can reveal pathologies such as celiac disease and pre-tumor or tumor lesions.
Preparation
How do you prepare for the exam?
The absence of food in the upper tracts of the digestive system guarantees better visualization and diagnostic accuracy. For this reason, it is advisable to keep fasting, avoiding ingesting food or drinks for at least 6-8 hours before the examination; the last meal before the gastroscopy must in any case be light and easily digestible (see in this regard the article on food digestion times). If gastroscopy is performed in the afternoon, a light breakfast is allowed, based on tea and rusks, or breadsticks by 7.00 am. It is advisable not to smoke before the examination.
Generally, it is not necessary to suspend the intake of any drugs that are taken as usual therapy; in this regard, please refer to the medical indications, given that, for example, it may be necessary to correct or possibly suspend therapies with oral anticoagulants (coumadin, sintrom), antiplatelet agents (aspirinette, ticlopidine or similar) or anti-inflammatory / painkillers (aspirin and the like). Before the examination, antacid drugs (such as maalox) or charcoal should not be taken.
Other conditions that may require special measures in view of an "esophagus-gastroduodenoscopy are valvular heart disease, the presence of pacemakers, immunosuppression and diabetes (with adjustment of the intake of oral hypoglycemic drugs and insulin before the" examination) .
On the day of the gastroscopy it is necessary to bring the health documents (referral, health card, etc.) and any clinical documentation (blood tests, previous endoscopic findings, radiological reports, etc.) to the clinic.
Immediately before the examination, the patient is informed of the procedures for carrying out the gastroscopy and of the risks of this investigation, requesting consent for the examination to be performed. During the interview, the patient will take care to inform the doctor or healthcare professional of any medical therapies in progress, allergies and adverse reactions to drugs, previous illnesses and any endoscopic examinations to which he has already been subjected. The woman of childbearing age must also warn of any or suspected pregnancy.
How is it done?
For a successful investigation, the patient should remain relaxed as much as possible. Generally, he is asked to lie down on his left side after anesthetizing the oral cavity with a spray or a candy to melt in the mouth; both can give the sensation of taste bitter, but they are important for numbing the throat and attenuating the gag reflex.
Before the examination, any removable dental prostheses (dentures) must be removed, as well as glasses, while electrodes and a bracelet will be applied to monitor vital parameters (blood pressure, heart rate). A protective mouthpiece will also be inserted between the teeth , to protect them and prevent the endoscope from being bitten.
In most cases, the patient is subjected to general sedation by intravenous injection of drugs, in order to make the gastroscopy more comfortable and increase the collaboration of the patient. While eliminating anxiety or at least significantly attenuating it, these drugs they do not completely sleep the patient, who remains able to respond to tactile stimuli and cooperate with verbal commands. Not infrequently, due to the effect of the drug, the patient forgets the experience or at least retains only a faded memory.
General anesthesia is very rarely used. If the patient prefers, esophagus-gastroduodenoscopy (EGDs) can also be performed without any sedation.
The examination begins with the introduction of the gastroscope into the oral cavity, which is then made to descend with extreme caution along the esophagus, up to the stomach and duodenum. At the gastric level, through the instrument, air will be introduced in order to stretch the walls and have a better view of them; inside, in fact, the gastroscope has channels that allow you to pass, if necessary, special micro-instruments, water or air.
A very sharp color image appears on the screen, with a high resolution of the inside of the stomach, and the ability to store snapshots and videos.
And "Painful?
By itself, gastroscopy is generally not painful and does not prevent breathing in any way; even the execution of any biopsies is not painful, since the mucosa has no nerves that perceive pain. However, especially in the absence of sedation, the examination still causes some discomfort, especially during the insufflation of air into the stomach. the descent of the gastroscope itself can cause a certain tension, with a sense of pressure on the abdomen, which at times can be unpleasant. oral in the esophagus, since voluntary swallowing - which facilitates the maneuver while minimizing discomfort - is generally associated with the appearance of a regurgitation stimulus.
The examination lasts about 15-20 minutes and can be prolonged if special interventions are required for unexpected results. If necessary, the sedative effect can be antagonized by another drug.
At the end of the gastroscopy it is possible, for a few hours, to feel a sensation of abdominal swelling which will disappear spontaneously. Other, usually mild, complaints may also be complained of, such as a hoarse voice.
After gastroscopy
At the end of the gastroscopy, the doctor will inform the patient about the outcome of the examination and will provide precise indications on the measures to be taken.
The use of sedative drugs during gastroscopy requires the most absolute abstention from driving and from the use of machinery in the 24 hours following the examination. For the same reason, in this period of time the patient will not have to sign documents with legal value or engage in other activities that require an important state of attention and full lucidity.
After about an hour from the gastroscopy, as soon as the sensitivity of the tongue and palate, as well as the swallowing reflex have been regained, the patient will be able to eat normally; a light meal, without alcohol, and rest for the rest of the day are recommended. a biopsy has been performed, the patient should avoid taking hot food, as this would increase the risk of bleeding.
If in the hours following the gastroscopy abdominal pain, dizziness, nausea) occur, or you notice the elimination of black and soft stools, it is important to contact your doctor or the nearest hospital immediately.
For what has been said, if the patient has been subjected to sedation, we reiterate the impossibility of returning home by personally driving the car, even in the absence of numbness and drowsiness.
Risks and complications
Is gastroscopy dangerous?
Gastroscopy is a safe and widely tested test. Only rarely can complications arise, the most common of which is stomach perforation, which on average occurs once in a thousand cases. The risk of complications is obviously greater in the case of operative gastroscopy (for example with biopsies), especially due to the risk of haemorrhages or wounds (perforations), further favored by particular anatomical conditions (esophageal stenosis, Zenker's diverticulum, neoplasms). Any bleeding is generally controllable endoscopically, and only in very rare cases may it require surgery or a blood transfusion.
Presence of pre-existing heart or lung disease can also increase the risk of complications. The risk of pneumonia secondary to the ingestion of aspirated material in the airways, and cardiac arrhythmias is limited, but not negligible. Other complications may be related to the type of sedation. More details about the complications can be requested from the endoscopist.
To protect the patient from the risk of transmission of infections, all accessories used during gastroscopy are disposable or subjected to sterilization, with particular attention to environmental hygiene.