In most cases, the cysts are small and harmless, while on other occasions they can be large and painful or, even worse, represent a sign of a malignant tumor of the ovary.
To establish the exact nature of an ovarian cyst, and to determine whether it is a benign or malignant tumor, a thorough gynecological examination and transabdominal or transvaginal ultrasound examination are required.
Less severe ovarian cysts do not require any treatment, as they heal spontaneously in a few weeks / months. Severe ovarian cysts, on the other hand, need to be surgically removed to prevent unpleasant consequences.
The gonads represent a fundamental part of the human reproductive system, as they are the glands that produce the gametes, or sex cells.
Two in number and bean-like in shape, the ovaries perform two functions:
- They secrete female sex hormones (estrogen and progesterone), which play an essential role in the development of secondary sexual characteristics and in reproduction.
- They produce the egg cell (or oocyte or oocyte), that is the female gamete. This cell is brought to maturity in the first half of the menstrual cycle, after which it is freed from the ovary (ovulation) and channeled into the fallopian tubes; there, it can eventually be fertilized by a sperm (male gamete).
Each ovary is located on either side of the uterus.
The uterus is the organ of the female genital apparatus responsible for receiving and nourishing the fertilized egg cell (ie the embryo first and the fetus later) for the whole period of pregnancy.
IS AN OVARIAN CYST ALWAYS A PATHOLOGICAL SIGN?
Over the course of life, a woman's ovary can develop one or more cysts, without causing any particular symptoms or problems. For this reason, unless they have certain characteristics, ovarian cysts are harmless and resolve spontaneously without need. of particular treatments.
EPIDEMIOLOGY
The appearance of ovarian cysts is a very frequent occurrence.
According to an Anglo-Saxon statistic, in fact, if a large number of women could be subjected to an ultrasound examination of the pelvic area at the same time, it would appear that almost all subjects of childbearing age, and at least 20% beyond menopause, have one or more ovarian cysts .
But how many of these women have symptoms or complaints related to cysts?
According to the same research, in their lifetime only 4 women out of 100 show problems related to the presence of ovarian cysts.
FUNCTIONAL CYSTS
There are 3 types of functional ovarian cysts:
- The follicular cysts. The egg cell is formed inside a protective structure, called the follicle. As soon as the egg cell is mature, therefore ready for a possible fertilization, a hormonal signal is triggered which determines the rupture of the follicle and the exit of the egg itself. in the direction of the fallopian tubes and the uterus. In some circumstances, this mechanism does not occur perfectly and the egg remains confined to the inside of the follicle, which fills with fluid and forms a follicular cyst. The follicular cysts are, by far, the most common ovarian cysts and almost never cause disturbances.Their resolution, which does not require any treatment, usually occurs within a few weeks (two or three menstrual cycles).
- Luteal cysts (or luteal cysts). The follicle, after having expelled the egg cell, takes the name of corpus luteum. Sometimes, the opening from which the egg cell has come out can close again, retaining fluids of various kinds and blood. On these occasions, a luteal cyst is formed. Luteal cysts, compared to follicular cysts, are less common but more dangerous: they can, in fact, rupture suddenly and give rise to painful internal bleeding.Their spontaneous resolution usually takes a few months.
Luteal cysts are particularly common during pregnancy. - Thecal cysts. Thecal cysts are formed from thecal cells that make up the follicle due to the effect of chorionic gonadotropin, a hormone produced during pregnancy. They are less common than both follicular and luteal cysts.
Follicular cysts
On average, they are about 2.5 cm in diameter
Luteal cysts
On average, they are about 3 cm in diameter
PATHOLOGICAL (OR NON-FUNCTIONAL) CYSTS
The main pathological (or non-functional) cysts are:
- The dermoid cysts. Dermoid cysts develop from the cells that produce the oocyte during embryonic life. For this reason, within them it is possible to trace portions of human tissues that resemble hair, bones, fat, teeth or blood. Dermoid cysts can assume important dimensions and even reach 15 centimeters in diameter; when the dermoid cyst is very large and causes an "alteration of the normal anatomy of the ovaries and uterus, surgery may be required to remove it. Dermoid cysts are benign tumors that very rarely become malignant.
They are the most common non-functional cysts among women under 40. - The cystadenomas. They are benign tumors that grow on the outer surface of the ovaries and which may contain (as a cyst) water or mucus. If they contain water, we speak of serous cystadenomas, while if they contain mucus we speak of mucinous cystadenomas.
Serous cystadenomas do not usually reach large sizes and do not cause particular disorders; mucinous cystadenomas, on the other hand, can grow considerably and even reach 30 centimeters in diameter.
A large mucinous cystadenoma can push on the adjacent intestinal tract or bladder, causing indigestion or frequent urination. in addition, it may rupture or obstruct the flow of blood to the ovaries.
The conversion of a benign cystadenoma into a malignant tumor is a very rare event.
They are the most common non-functional cysts among women over 40. - Cysts due to endometriosis (or endometriomas). Endometriosis is a disease characterized by the presence of endometrial tissue outside its natural site, which is the uterus. In some women, however, it can also be characterized by the appearance of ovarian cysts filled with blood.
- Cysts due to polycystic ovary syndrome. Polycystic ovary syndrome (or polycystic ovarian syndrome) is a morbid condition characterized by enlarged ovaries covered with many small cysts. Its appearance is usually caused by an imbalance in the production of ovarian (ie produced by the ovaries) and pituitary (ie produced by the pituitary) hormones.
- Pelvic pain. It can be deaf if the ovarian cyst is large but still intact, or sharp and sudden if the ovarian cyst has ruptured. Sometimes, the painful sensation is also felt in the back and thighs.
- Pelvic pain during sexual intercourse.
- Difficulty completely emptying the intestines.
- Need to urinate often. It is due to the fact that the ovarian cyst constantly presses on the bladder.
- Changes in the normal menstrual cycle.
- Sense of heaviness and swelling in the abdominal area.
- Recurrent indigestion and a sense of fullness even after light meals.
- Dizziness, vomiting and a feeling of emptiness in the head.
- Sense of persistent tiredness.
WHEN TO SEE THE DOCTOR?
If a woman experiences the aforementioned complaints (in particular pelvic pain accompanied by a sense of vomiting), she should contact her doctor immediately, to arrange a check-up. Although dangerous ovarian cysts are infrequent, it is in fact better not to take risks and to resort to all the necessary precautions.
COMPLICATIONS
The complications related to the presence of ovarian cysts are due to their rupture (which can give rise to an "internal hemorrhage) and to the twisting of the ovaries (because the latter" receive little blood).
(ie that do not cause symptoms or disorders) goes unnoticed (so the patient does not notice) or is diagnosed by chance, after a pelvic exam or a "routine ultrasound scan.When the cysts are symptomatic, it is advisable to always investigate the nature of the problem and undergo a specialist check-up at a gynecologist.
GYNECOLOGICAL VISIT AND SPECIALIST EXAMINATIONS
During the gynecological examination, the doctor asks the patient to describe the symptoms in progress, investigates their clinical history, evaluates any suspicious ultrasound scans and performs an accurate vaginal examination.
If the patient has not yet undergone an ultrasound, the gynecologist will certainly prescribe it. In addition, he will prescribe a specific blood test for the tumor marker CA125.
Ultrasound. Two types of ultrasound can be performed: transabdominal and / or transvaginal. Transabdominal ultrasound is performed by passing the ultrasound probe over the patient's abdomen; in this way it shows both the uterus and the ovaries, but it is not always exhaustive.

Figure: appearance of a 2 cm ovarian cyst on ultrasound examination. From the site: en.wikipedia.org
The transvaginal ultrasound, on the other hand, is performed by introducing the ultrasound probe inside the vagina; in this way, it shows in detail the pelvic organs of interest.
Blood tests and specific search for the tumor marker CA125. Ovarian cysts formed as a result of a malignant tumor process are characterized by the high presence, in the blood, of a protein called CA125. Therefore, with a specific blood test, the doctor measures the levels of CA125, to be sure of the exact nature of the ovarian cyst found.
However, it should be noted that a high level of CA125 is not always due to a malignant ovarian cyst: for example, it can be connected to completely different pathologies, such as endometriosis, pelvic inflammatory disease or tuberculosis.
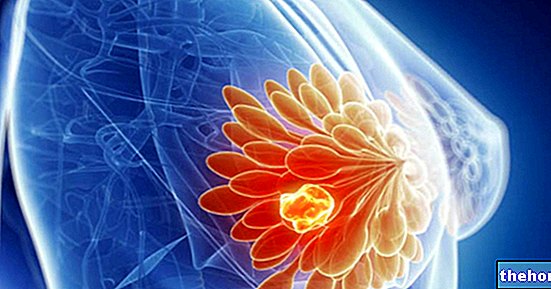
What features of the ovarian cyst are of interest to the gynecologist?
The shape: is it irregular or not?
The size: the presence of symptoms is linked to the size of the cysts
The composition: Does the cyst contain liquid or solid material? Or both? The presence of solid matter could mean that the cyst is malignant, therefore further tests must be carried out.
If no improvement is observed, then surgery should be considered.
SURGERY: WHEN AND HOW TO INTERVENE?
An ovarian cyst must be removed by surgery if:
- It is of an important size
- It causes severe symptoms
- It is malicious or there is a strong suspicion that it is
If the cyst is benign and the patient is still of childbearing age, the operation will only affect the cyst (ovarian cystectomy); on the other hand, if the cyst is very large or perhaps malignant or if the patient is no longer fertile (therefore she has passed menopause ), then the operation will involve the entire diseased ovary (oophorectomy).
There are two surgical techniques available to the operating physician:
- Laparoscopy. Reserved for patients with benign cysts of a significant but not excessive size, laparoscopy is a minimally invasive surgical procedure, ideal for ovarian cystectomy operations.
- Laparotomy. Indicated for patients with very large and / or malignant (or presumed) cysts, it is a highly invasive surgical procedure, as the surgeon, in order to completely remove the cyst, must make an "important incision on the belly.
In general, the removal involves the entire ovary, although in cases of benign tumor it is possible to limit itself to the elimination of the cyst alone.
Once the operation is complete, the incision is closed with sutures.
The diseased ovary (if removed due to a suspected malignant tumor) is delivered to a doctor specialized in pathology, for laboratory analysis. The latter (if they confirm the presence of a malignant tumor) allow to establish the degree of malignancy cancer and chemotherapy therapy to be adopted.
Recovery times for an ovarian cystectomy. Laparoscopic surgery 2 weeks Laparotomy surgery 6-8 weeks
On what occasions are bilateral oophorectomy and hysterectomy performed?
The presence of a malignant ovarian cyst requires surgeons to remove, in addition to the diseased ovary, also the healthy ovary (bilateral ovariectomy) and the uterus (hysterectomy). This double operation is highly invasive and definitively compromises the fertility of a woman not yet in menopause (therefore potentially still able to conceive).
For women of childbearing age who are subjected to the removal of the ovaries and uterus, we speak of "surgical menopause".
In depth: when to contact your doctor after surgery?
After a laparoscopy or laparotomy surgery, it is quite normal to feel pain in the pelvic area.
It is not normal, however, that:
- The painful sensation gets worse rather than better
- Severe blood loss occurs
- The patient has a high fever
- A malodorous liquid comes out of the patient's vagina
If you have one or more of these symptoms, you should contact your doctor immediately.
WHAT TO DO IN CASE OF SEVERE PAIN?
In case of severe pain in the pelvic area, the doctor recommends taking painkillers, such as acetaminophen, and anti-inflammatories, such as NSAIDs (ibuprofen).
It also points out some soothing remedies, such as applying a hot water bottle to the stomach or taking hot baths.