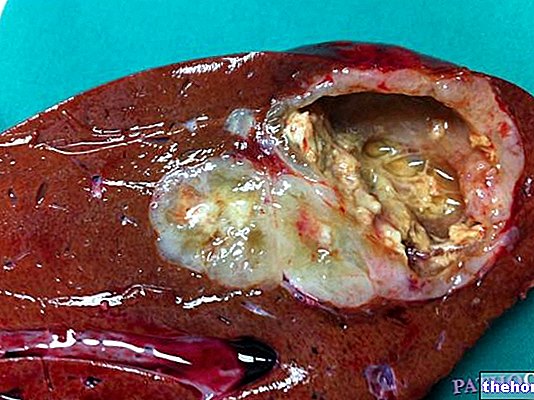
The duodenal ulcer is a lesion of the mucosa that lines the initial part of the small intestine internally, called the duodenum. It is a real erosion, in the shape of a crater, which can be more or less deep. The formation of a "duodenal ulcer is often linked to an" excessive production of acid by the stomach; when these acidic juices are poured into the intestine, they are partly buffered by the intestinal digestive juices. However, if the acidity is excessive, the walls of the duodenum can be damaged and an ulcer can form. Excessive acidity of stomach contents may be due to genetic factors, stress, smoking or the use of anti-inflammatory drugs, such as cortisone and aspirin. In addition to the problems of gastric hyperacidity, duodenal ulcer is often linked to infection with Helicobacter pylori. It is a very particular bacterium, as it is capable of proliferating in the acidic environment of the stomach; the presence of this bacterium alters the protective layer that protects the mucous membranes of the stomach and duodenum from acids; consequently, it favors the appearance of gastritis and peptic ulcers. In addition to creating various symptoms and ailments, over time a duodenal ulcer can lead to very serious complications, including bleeding, perforation or narrowing of the duodenum, which is why it must be treated promptly.
We have already said that duodenal ulcer often develops due to excess hydrochloric acid produced by the stomach and poured into the duodenum. However, another substance present in the gastric juices, called pepsin and involved in the digestion of proteins, can also contribute to the formation of a duodenal ulcer. I remind you that the walls of the stomach and duodenum are normally protected from acid juices, thanks to a layer of mucus that lines the mucosa. However, for various reasons, this defense can be compromised. The duodenal ulcer is therefore the result of an imbalance between aggressive factors, such as acidity of gastric juices, and protective factors, such as mucus, which defend the duodenal mucosa. Today we know that most duodenal ulcers are caused by an infection. The manager, as already mentioned, is theHelicobacter pylori, a microorganism capable of living in the acidic environment of the stomach. Once this bacterium has entered the body, it causes an inflammatory reaction that can damage both the walls of the stomach and those of the duodenum. The acid and enzymes produced by the stomach can thus more easily reach the underlying tissues and damage them to the point of causing an ulcer. Among the other possible causes of duodenal ulcer we remember the continuous use of some gastrically damaging drugs, such as aspirin or cortisone. There are also numerous other predisposing factors that can favor the onset of a duodenal ulcer. abuse of alcohol or coffee, smoking and certain wrong eating habits. Duodenal ulcer mainly affects men, with three times the frequency of women. Furthermore, unlike gastric ulcer, duodenal ulcer recognizes a familial predisposition.
The most characteristic symptom of duodenal ulcer is the appearance of a pain localized to the upper region of the abdomen, between the lower extremity of the sternum and the navel. It is a burning, dull and continuous pain, which appears especially in the stomach. empty, often one to three hours after main meals, or during the night, causing awakening. The pain typically subsides by ingesting food, which in this case has a buffering effect. In other cases, the pain has less specific characteristics .
Sometimes, duodenal ulcer can be accompanied by other symptoms, such as loss of appetite, abdominal swelling, nausea and vomiting. Another characteristic aspect of ulcer is seasonality: if left untreated, it tends to recur periodically, worsening mostly in spring and autumn.
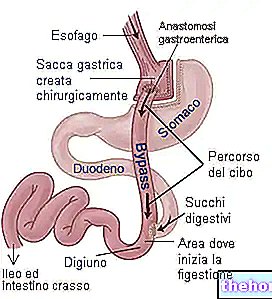
Complications of duodenal ulcer arise when erosion perforates the mucosa and extends deeply. For example, the ulcer can reach the underlying blood vessels triggering actual bleeding. The bleeding can cause anemia or, if it occurs acutely, it can become evident through the emission of blood through vomit or stool; in the presence of a "gastric or duodenal haemorrhage, the faeces, in particular, take on a blackish color, similar to tar. In extreme cases, the ulcer can extend to the full thickness of the duodenum, perforating its wall. The resulting leakage of intestinal contents can cause infection or injury to nearby organs, such as the liver and pancreas. For this, a perforated ulcer is a life-threatening condition requiring immediate medical-surgical treatment. Perforation of a duodenal ulcer may be signaled by the onset of sudden, excruciating pain associated with vomiting containing digested blood. Another possible complication of duodenal ulcer is the narrowing of the duodenum, called duodenal stenosis; this occlusion is linked to an excessive deposit of scar tissue produced to repair ulcerative lesions.
The most used tests for the diagnosis of duodenal ulcer are "endoscopy, radiography with bariate contrast medium and the search for infection by Helicobacter pylori. The first examination is called gastroduodenoscopy and is based on the use of a small probe equipped with a camera, which is made to go down through the patient's mouth. In this way the camera transmits images of the duodenal lesions and allows to evaluate the health of the duodenum. the same examination also allows the removal of small fragments of tissue to be subjected to histological examination under the microscope. In this way it is possible to assess the type of cell damage with greater accuracy and it is also possible to highlight any infection by Helicobacter pylori. The latter can also be assessed by simpler tests, such as stool or blood tests and the so-called breath test.
It is possible to relieve the symptoms of duodenal ulcer by avoiding smoking, alcohol and drugs that aggravate the ulcer. The treatment also begins with a healthy and correct diet. In particular, it is a good idea to give up large meals and coffee, tea, chocolate, mint, carbonated drinks, cold cuts, spicy foods and fried foods. Speaking of drugs, antacids, histamine H2 receptor antagonists and proton pump inhibitors are often recommended to neutralize gastric acidity. In case of infection with Helicobacter pylori, these drugs must be combined with antibiotic treatment to eliminate the infection. Surgical therapy, finally, is reserved for the most serious cases and for the treatment of complications such as haemorrhages, perforations or stenosis.