In the previous video-lesson we talked about ulcerative colitis; today we will get to know more closely another important inflammatory bowel disease, which unlike the previous one can affect not only the colon and rectum, but also other sites of the digestive system. I'm talking about Crohn's disease.
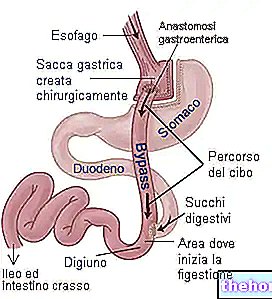
Crohn's disease is a chronic inflammatory disease that affects the digestive system; in most cases it affects the last part of the small intestine, called the ileum, and the colon, however it can potentially affect any part of the digestive system. , from the mouth to the anus. The inflammatory process that characterizes Crohn's disease is accompanied by "segmental" and discontinuous lesions; this means that these lesions are present only in some tracts of the digestive tract, which are interspersed with other segments entirely In the diseased tract there are inflammation, swelling and ulcers that affect the entire thickness of the intestinal wall. For this reason, perforations or fistulas can be created, that is, abnormal passages between the intestine and other nearby organs. Crohn's are not yet fully known. It is hypothesized that autoimmune reactions are at the basis of the disease, probably triggered by previous and intestinal infections or from genetic or environmental factors, such as diet or the use of particular drugs. Symptoms that accompany Crohn's disease include abdominal pain, diarrhea with or without blood in the stool, nausea, fever, weight loss, and general malaise. The disease has an intermittent course, with the characteristic tendency to "rekindle" in acute attacks alternating with periods of well-being. Over time, intestinal damage can cause digestive complications and more. To give an example, the inflammatory process can cause difficulties in assimilating food or even narrowing of the intestinal wall, up to occlusion. In general, drug therapy with anti-inflammatory and immunosuppressive agents allows control of Crohn's disease and its progression. In cases where this approach is not sufficient, it is instead necessary to resort to surgery.
Crohn's disease is a disease of unknown origin, in the sense that the triggering causes are not yet well defined. Currently, it is believed that genetic, environmental, immunological and dietary factors can predispose to the chronic inflammatory process underlying the disease. Viral and bacterial infections have also come under fire over the years, but the evidence confirming this theory is uncertain. Similarly, it has been hypothesized that there is a "genetic hypersensitivity of the immune system to stimuli normally present in the digestive system; specifically, particular dietary molecules or components of the microbial flora would determine a" hyperactivation of the immune system, which would turn against the same cells in the body damaging the digestive tract involved. This would trigger an inflammatory reaction and all the damage and symptoms associated with Crohn's disease. In these genetically predisposed individuals, factors such as smoking, a diet high in refined sugars and low in fruit and vegetables, can play a decisive role in favoring the onset of the disease. In support of this statement, it should be noted that Crohn's disease is constantly increasing in industrialized countries, while it is practically almost unknown in the third world. disease can occur at any age; however, it tends to present yes, especially in adolescents, in the twenties and in the age group between 50 and 70 years.
The symptoms with which Crohn's disease occurs depend on the location, extent and aggressiveness of the disease process. Abdominal pain and diarrhea may be present, characterized by 2 to 10 diarrheal discharges per day sometimes mixed with blood and mucus. Malabsorption, nausea and vomiting, weight loss, weakness and generalized malaise are also often observed. In addition to intestinal manifestations, rashes, oral lesions, pain in the joints, inflammation of the eyes can arise, and as for children, there may be a delay in growth. In addition to being a disease with a chronic course, Crohn's disease is also relapsing, so it intersperses periods of relative normality with others of exacerbation lasting days or weeks. If not properly treated, Crohn's disease can lead to stenosis, that is, narrowing of the intestine with the risk of occlusion, and the appearance of abscesses or fistulas, especially around the anus. Additionally, Crohn's disease increases the risk of colorectal cancer.
From a diagnostic point of view, Crohn's disease can be suspected in the presence of characteristic symptoms; this suspicion is strengthened when blood tests show an increase in inflammatory indices. I am referring, in particular, to the increase in the erythrocyte sedimentation rate (known as ESR) and in the C reactive protein (or PCR). In order to dispel any doubts and reach a definitive diagnosis, it is however necessary to resort to instrumental investigations; among these we remember the double-contrast opaque colon enema, intestinal ultrasound and above all colonoscopy. This last survey, in particular, allows you to visually appreciate localized inflammation and the possible presence of superficial and deep ulcers. Not only that, during the examination there is the possibility of carrying out biopsies by taking small tissue samples; after which, by analyzing these samples under the microscope, the doctor will be able to assess the presence of typical aspects of chronic inflammation and thus reach a definitive diagnosis.
At present, Crohn's disease is not curable. However, there are a number of therapeutic approaches available to control symptoms and prevent the disease from worsening. The aim of the treatment is to obtain longer periods of remission and less intense acuity. To achieve or maintain this result, depending on the severity of the inflammatory process, more or less powerful anti-inflammatory drugs are used, such as aminosalicylates and corticosteroids; among the first we remember sulfasalazine, mesalazine and "olsalazine; among the cortiscosteroids I remember prednisolone and deoxymethasone. In combination with anti-inflammatories, antibiotics and immunosuppressive drugs can also be administered, which attenuate the body's immune reactions and block the In recent years, therapies with biological drugs have also been introduced, such as antibodies that selectively block TNF-alpha, one of the main molecules involved in the inflammatory process. This is the case of infliximab and adalimumab, which for the potential side effects are typically used only if other drug approaches fail. In cases refractory to drug therapy or when the disease is complicated, surgery is used which generally involves resection of the intestinal tract affected by the disease. It should be noted, however, that this type of intervention does not definitively cure the disease, which can reappear in other intestinal segments.