In the "last video we began to learn about cystitis, focusing on the most common form, which is that of an infectious nature. We also mentioned that cystitis can be favored by various triggers and that it is not always possible to identify a precise cause. Interstitial cystitis, also called painful bladder syndrome, is one of the typical cases in which the origin of cystitis is uncertain. Let's see together what it consists of.
Interstitial cystitis is one of the most complex pathologies in the urological field. We are talking about chronic inflammatory bladder disease, which can be extremely debilitating. Interstitial cystitis, in fact, causes numerous problems, ranging from the almost constant need to urinate to the pain associated with each urination. All this in the absence of infections or other demonstrable bladder pathologies.
As anticipated, therefore, the underlying cause of this bladder inflammation is currently unknown, although infectious, hormonal, vascular, neurological or secondary origins to an immune pathology have been proposed. In addition to autoimmune disorders and recurrent urinary tract infections, sexually transmitted diseases, allergies to drug treatments and trauma, including surgical, in the pelvic area have also been hypothesized among the possible causative factors of interstitial cystitis. Often the causes are multiple and this is why interstitial cystitis is considered a multifactorial pathology.
Interstitial cystitis can affect people of any age or gender. However, it occurs more frequently in women between the ages of 20 and 50.
In addition to the difficulties in identifying a precise triggering cause, interstitial cystitis is a disorder that is still difficult to diagnose today. Sometimes, in fact, the bladder seems absolutely normal, although the patient complains of discomfort and severe pain. the fact that interstitial cystitis is a difficult pathology to cure. The only good news is that, fortunately, its occurrence is rare.
Interstitial cystitis presents with the same symptoms as the “classic” infectious cystitis, therefore with burning and pain during the emission of urine, pelvic pain and bladder filling, and an urgent and frequent urge to urinate. However, there are no signs of urinary infection, the microbiological analyzes are negative and taking antibiotics does not lead to any improvement.
Returning to the symptoms, in women, the disorder is often associated with vaginal pain, such as to make it impossible to have sexual intercourse. Men with interstitial cystitis, on the other hand, can suffer from pain in the testicles, scrotum, and perineum, as well as having painful ejaculations. Interstitial cystitis is also characterized by alterations of the bladder wall, detectable with cystoscopy and histological investigations, which we will discuss later in the video.
In addition to the symptoms already listed, some patients also report having muscle and joint pain, migraines, various forms of allergy and gastrointestinal problems. Going into more detail, it also seems that interstitial cystitis is associated, in a way not yet well understood, with some chronic conditions such as fibromyalgia, irritable bowel syndrome and other painful syndromes. However, many patients with interstitial cystitis have only occasional or constant bladder symptoms.
For most people with interstitial cystitis, it is not at all easy to arrive at a diagnosis of the disorder. We could say that this is basically based on the exclusion of other diseases and conditions that have similar symptoms. Diagnosis must therefore exclude bacterial cystitis, bladder cancer, kidney disorders, urinary tuberculosis, vaginal infections and sexually transmitted diseases, endometriosis, cervical, uterine and ovarian cancer, prostatitis, prostate cancer and neurological disorders.
To reach a certain diagnosis of interstitial cystitis, the urologist must resort to accurate diagnostic tests, including urine culture and cystoscopy; the latter is an endoscopic examination of the bladder, which is performed under general or local anesthesia, in order to assess the state of the organ.
We have already seen that urine culture is necessary for the search for bacteria in urine. In fact, starting from the consideration that common cystitis is often caused by a bacterial infection, the responsible pathogen is discovered through urine culture. Therefore, if the patient presents typical symptoms of cystitis, but almost sterile urine emerges from the urine culture, it is probably precisely interstitial cystitis.
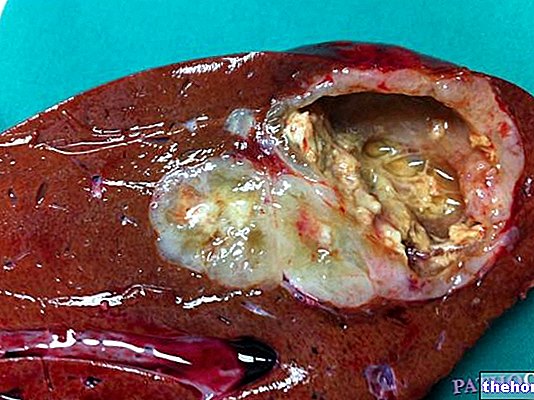
If there is no infection and no other pathology is detected, the doctor may resort to a cystoscopy with hydro-distension of the bladder; in practice, physiological saline solutions are injected into the organ, to allow a better vision of the bladder mucosa. The distension of the bladder during the investigation is particularly useful because it allows to highlight a characteristic picture. irritation of the bladder mucosa, at the level of which numerous small dark red spots may be present, similar to petechiae, sometimes ulcerated.These lesions, called Hunner's ulcers, when present, are diagnostic for interstitial cystitis.
At this point, a biopsy of the bladder wall may be necessary for definitive confirmation. In practice, a small sample of tissue is taken to be examined later under the microscope. This examination, called histological, typically reveals an inflammatory infiltrate typical of interstitial cystitis, with immune cells and tissue glomerulations, in the absence of infections or other pathologies.
Unlike "common" bacterial cystitis, interstitial cystitis does not respond to conventional antibiotic therapy. It should also be emphasized that to date there is no specific and decisive treatment for the disease. However, various pharmacological, physical or surgical measures are available, aimed at reducing inflammation and discomfort in the bladder. In any case, the results are highly variable from patient to patient.
Oral drug therapies include the prescription of painkillers, anti-inflammatory drugs and tricyclic antidepressants, such as amitriptyline. Other oral medications intended for the treatment of interstitial cystitis are sodium pentosan polysulfate and some antihistamines, such as cimetidine.
Another therapeutic approach consists in instilling directly into the bladder drugs with reparative capacity against the bladder mucosa, such as dimethyl sulfoxide and heparin.
Other therapeutic interventions are represented by the bladder instillation of hyaluronic acid, the injection of botulinum toxin, transcutaneous electrical neurostimulation or TENS, etc. Finally, surgery can be considered in extreme cases, which do not respond to traditional treatments.
Ultimately, the treatment of interstitial cystitis is a specialist competence. The choice between the various treatment modalities must therefore be made on the basis of the individual case, often combining different interventions.
As for behavioral measures, even nutrition can aggravate the problem of interstitial cystitis. Very spicy or irritating foods, such as spices, citrus fruits, tomatoes, chocolate, sausages, alcoholic beverages, and coffee, can make the existing ailment more serious. It is therefore important to eat healthily, trying to reduce or eliminate foods that can cause irritation and inflammation of the bladder. Finally, particular attention is paid to the correction of any postural anomalies, and to the adoption of a healthy lifestyle, with optimal management of daily stress and regular physical activity.




.jpg)