Today we will get to know more closely a bowel disease quite frequent in industrialized countries, especially among the elderly. I'm talking about the inflammation of the intestinal diverticula, which in medical terms is called diverticulitis. In this episode we will see together what diverticula are, why they form and why they sometimes become inflamed, triggering diverticulitis.
Before going any further, the difference between diverticulitis and diverticulosis must be understood, as the two conditions are often confused. Hence, diverticulosis is simply a disease characterized by the presence of diverticula. On the other hand, we speak of diverticulitis when these diverticula become inflamed. Diverticulitis, therefore, is a complication of diverticulosis. In general, remember that whenever you come across the suffix -ite in a medical term, such as tendonitis, gastritis, esophagitis, pulpitis and so on, it means that this term refers to an inflammatory process.
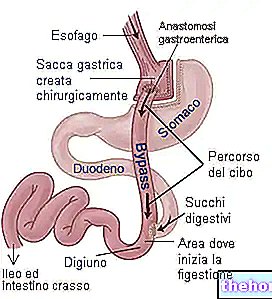
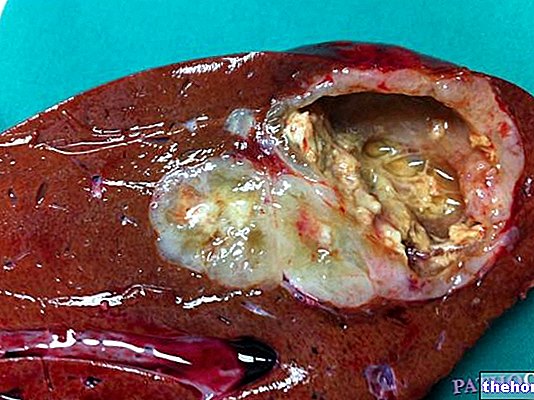
But what are diverticula? Diverticula are protrusions that form along the walls of the intestine. In practice, they are like small pouches of the intestinal mucosa and submucosa, which appear as rounded protrusions. In diverticulosis, as you can see in the image, instead of being smooth, the wall of the intestine therefore has grooves, pockets that deepen towards the outside. The dimensions of the diverticula can vary from that of a pea to that of a marble. Moreover, they can be single, even if very often they are multiple. Before seeing the next slide, it is important to underline that the whole digestive tract can be home to diverticula; I remember for example the esophageal diverticula, therefore of the esophagus, but also the gastric ones and duodenals. In any case, the colon, that is the last part of the intestine, is the portion of the digestive tract in which their presence is most common.
Let us now examine in more detail what causes can determine the formation of diverticula. First, there is an anatomical reason why diverticula are more common in the colon. In the colon, in fact, the blood vessels penetrate along the entire thickness of the intestinal wall, creating areas of less resistance. In these points where the intestinal wall is weaker, the formation of diverticula is therefore more likely. Another extremely important factor in the appearance of diverticula is the increased pressure within the intestinal lumen. The increase in pressure inside the intestine, in fact, causes the colon wall to become tired in the long run, paving the way for the appearance of diverticula. As we can easily guess, intestinal pressure increases as the internal content of the bowel increases. For this reason, the disease is related to constipation, and therefore to the prolonged stagnation of stool inside the colon. In turn, constipation is related to a diet low in liquids and dietary fiber. The fibers, in fact, stimulate the motility of the intestine and make the stool softer and easier to eliminate. Consequently, the fibers facilitate both the transit of stools along the intestinal lumen and the reduction of pressure in the colon. In a person who consumes a diet low in liquids and fibers, generally the stools are hard and compact; the intestine consequently has to contract more to expel them, and the pressure inside it increases accordingly. In addition to constipation, diverticulosis of the colon is favored also by a certain genetic predisposition and is often related to obesity. The incidence of diverticulitis progressively increases with age, so it hardly strikes before the age of 40 and is more frequent in people over the age of 60. Given the predisposing factors, it is not surprising that diverticulosis and diverticulitis are more common in industrialized countries. and increasing in the younger sections of the population, increasingly prone to obesity problems.
Generally, the presence of diverticula does not cause any discomfort; however, it may happen that these diverticula become inflamed causing the onset of diverticulitis. This condition manifests itself with abdominal pain, fever, nausea, spasms, and sometimes bleeding. In severe cases, the inflammation of the diverticula can cause various possible complications, such as the formation of abscesses, intestinal obstructions or perforations with consequent peritonitis. Having clarified this, however, it remains to be clarified why diverticulosis can become complicated in peritonitis. You should know that diverticula tend to become inflamed when food residues accumulate inside them or fecal material stagnates. By remaining trapped inside the diverticulum for a long time, this material becomes fertile ground for some bacteria, which normally populate the intestine without creating problems. The consequent overgrowth of these microorganisms can, however, become harmful and trigger an "inflammation of the diverticulum. Data to the hand, inflammation of the diverticula occurs in 10 to 25% of people with diverticulosis.
The risk factors for diverticulitis are basically of two types. The first of these is related to the disease. I mean that if the diverticula are very numerous or large then they are also more likely to become inflamed. The second risk factor we have already seen and is related to the transit of feces through the colon. In fact, I remember that if the stools are of hard consistency, intestinal transit is difficult or slowed down; this can favor both the formation of diverticula and their inflammation. A reduced water intake and a high-fat, low-fiber diet are therefore predisposing factors for both diverticulosis and diverticulitis. At this point, however, an important aspect must be specified and that is that in the presence of diverticulosis the inflammation of the diverticula can be favored not only by a diet low in waste, but also by some foods rich in fiber. The greater risk would be related to the consumption of foods that leave a large fibrous residue inside the colon, such as fruit or vegetables rich in seeds and nuts; especially in case of constipation and large diverticula, these residues could in fact accumulate in the diverticular pockets, facilitating inflammation . In any case, it is more a question of traditional suppositions and advice, which do not seem to have an effective experimental and scientific confirmation.