Let's get to know hepatitis C more closely, considered one of the most serious infectious diseases affecting the liver. During the lesson we will try to understand together the reason for this statement.
The virus responsible for hepatitis C (also called HCV, from the English Human Hepatitis C virus) is transmitted mainly through the blood of an infected person. Once it enters the body, this virus attacks the liver, causing inflammation. L hepatitis C can manifest itself in the form of acute hepatitis, but in most patients it is asymptomatic or presents with mild and not very specific symptoms, simulating a "passing flu". Despite this apparently reassuring aspect, in a large percentage of cases, estimated up to 85%, hepatitis C continues to gradually undermine the health of the liver. This means that the infection can go unnoticed and the virus can thus persist in the liver, continuing to seriously damage it to the point of making organ transplantation necessary in the most extreme cases. Not only. In addition to evolving into a long-lasting disease, chronic hepatitis C, after many years can lead to liver cirrhosis and liver cancer.
The hepatitis C virus, as we have just seen, is mainly transmitted through the blood of an infected person. Infection through the blood, therefore, can be facilitated by the sharing of syringes for intravenous drug inoculation, but also by the use of inadequately sterilized medical or aesthetic instruments. Blood transfusions represented the prevalent risk factor for the spread of the pathogen until the 1990s. However, after the introduction of mandatory blood screening, the incidence rate of transfusion-associated hepatitis C has almost disappeared. Infrequent, but still possible, is the transmission of the infection through unprotected sexual intercourse. the risk is, however, the relationships between homosexual men, especially if they are HIV positive. As with many other sexually transmitted diseases, in fact, the risk of contagion increases if there is exposure to blood, such as in energetic sexual intercourse, in anal intercourse, in fisting or in sex during the menstrual cycle. Finally, hepatitis C can be transmitted vertically, that is, from an infected mother to her child during pregnancy or childbirth.
Hepatitis C has a fairly long average incubation period; on average it is 5-10 weeks, with an interval ranging from 2 weeks to 6 months. As mentioned in the previous slide, most people with hepatitis C do not experience any symptoms or have vague and non-specific manifestations, therefore easily confused with those of other pathologies. In fact, many people do not realize that they have contracted hepatitis C, at least until, years or even decades after the infection, significant liver damage emerges. Remember, in fact, that the greatest risk associated with hepatitis C is the chronicity of the disease itself. In other individuals, during the early stages of hepatitis, generalized malaise, weakness, fever, vague abdominal discomfort, nausea, loss of appetite, muscle and, sometimes, joint pains occur. In some cases, jaundice appears, which we remember is the yellowish color of the skin and ocular sclerae. In the acute stage, a fulminant and fatal course is observed very rarely.
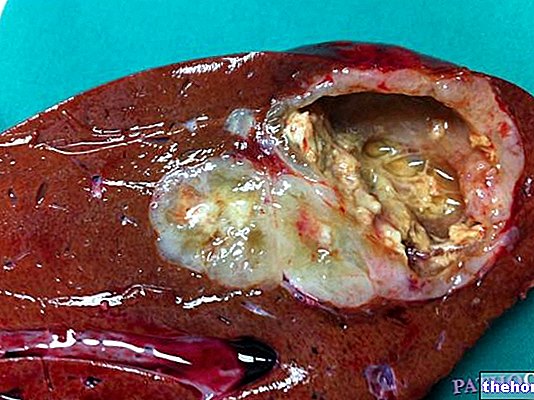
According to medical statistics, about 20-30% of people with acute hepatitis C recover completely. However, we have repeatedly highlighted how the most frequent and fearful complication is represented by the chronicization of the infection. In the initial stages, even for many years, chronic hepatitis C is often associated with non-specific symptoms, including a state of fatigue and persistent malaise. After many years, approximately 15-30 from infection, chronic hepatitis can progress to liver cirrhosis. Cirrhosis is the result of the continuous repair of liver tissue damage caused by the virus; this process leads to fibrosis, ie the formation of non-functional scar tissue in place of the healthy one. The progressive extension of fibrosis leads to liver failure, in practice the liver is no longer able to perform the functions required by the body. In addition to causing many complications, liver cirrhosis can facilitate the development of the most serious and fearful complication of hepatitis C. I refer to liver cancer.
The diagnosis of hepatitis C is based on the search for viral RNA and antibodies directed against the antigens of the virus. Therefore, it is sufficient to take a blood sample, to be subjected to various serological and molecular tests. The polymerase chain reaction (called PCR), in particular, allows the quantification of circulating viral RNA, which is an index of active infection. In addition, it allows the identification of the responsible viral genotype. On some occasions, blood tests carried out to look for a possible liver problem reveal persistent changes in some liver enzymes, such as high transaminases. In this case, it is good practice to continue investigations to exclude or confirm hepatitis C virus infection. In addition, if the doctor suspects severe liver function impairment, he may suggest performing a liver biopsy to ascertain more precisely the extent of the damage caused by the virus.
As we have seen, in rare cases, the infection can resolve itself without the need for any therapy. On the other hand, when hepatitis C becomes chronic, as happens in most cases, the treatment involves the combination of two antiviral drugs, called pegylated interferon alfa and ribavirin.This therapeutic protocol allows to inhibit the replication of the virus and to limit liver damage. Clearly the protocol will be customized by the doctor and possibly modified to suit the individual case. The effectiveness of therapy with alpha interferon and ribavirin is conditioned by both the characteristics of the virus and those of the host. Overall, these drugs are able to effectively counteract hepatitis C in about 50-80% of treated patients, especially if therapy is started early. Those who unfortunately develop cirrhosis or liver cancer, on the other hand, may need a liver transplant. Regardless of the therapeutic protocol adopted by the doctor, the abstention from alcohol consumption and the adoption of a sober diet without excesses is always strongly recommended. Furthermore, always under medical advice, particular attention should be paid to the use of drugs potentially toxic to the liver, such as paracetamol.
To date, although several trials are underway, a vaccine that protects against the hepatitis C virus is not yet available. The lack of a vaccine is mainly due to the variability of the surface proteins of the virus, against which it is not possible to obtain effective antibody protection. The only way to prevent infection is to comply with general hygiene rules and avoid risk factors as much as possible. Prevention therefore consists in the use of disposable syringes and avoiding the exchange of personal hygiene items, such as toothbrushes, scissors and razors. Also, anyone who decides to get a piercing or tattoo should make sure that the tools used are sterilized. Finally, as we have seen, in certain circumstances, hepatitis C can also be transmitted through sexual contacts, which can cause injury. It is therefore essential to respect the first rule of safe sex, that is to use condoms correctly during sexual intercourse, especially when it is occasional.

.jpg)