Hemorrhagic cystitis is an "acute inflammation of the bladder, very similar to the classic infectious form, but distinct from it precisely because of its hemorrhagic nature, therefore associated with blood loss.
In haemorrhagic cystitis, blood loss is the expression of damage to the inner lining of the bladder and the underlying blood vessels. For this reason, haemorrhagic cystitis is characterized by the presence, to a greater or lesser extent, of blood in the urine.
Hemorrhagic cystitis can arise from various causes. Usually, it is caused by a "bacterial infection, especially in young women. More rarely, it is induced by drugs, radiation, reactions to toxic substances, or pre-existing urogenital diseases."
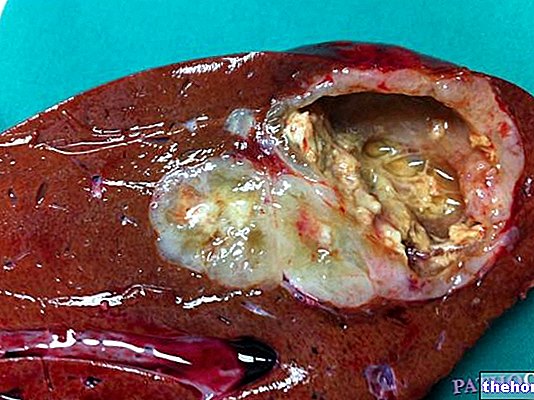
The term cystitis indicates an "inflammation of the urinary bladder. This last" - which as we know is the organ responsible for accumulating urine (produced by the kidneys), before eliminating it from the outside - is a hollow organ, whose wall is made up of four superimposed layers of tissue. From the inside to the outside, these layers take the name of: mucosa, submucosal, muscular and serous.In hemorrhagic cystitis, the acute inflammatory process affects the mucosa, the submucosa and the network of capillaries that irrigate them. It is precisely the involvement of the capillaries that determines the hematuria, that is the loss of blood with the urine. In other words, the inflammation reaches the capillaries, causes their congestion and damages them. The capillaries, therefore, can break, causing a "hemorrhage that is evident in the urine. Therefore, in addition to presenting the same symptoms of normal acute cystitis, in hemorrhagic cystitis there is also a certain loss of blood in the urine. Consequently, if the bleeding is copious the urine is bright red, while it assumes a pink or purplish color if the blood is present in the urine in less quantity.
Let's now see together what are the possible underlying causes of the disorder.
First of all, the various causes of hemorrhagic cystitis can be grouped into two large groups, those of an infectious nature and those of a non-infectious nature.
As for the infectious form, in most cases it is an infection caused by bacteria, such as Escherichia coli and Staphylococcus saprophyticus. At other times, fungal infections, such as cystitis caused by Candida albicans, may be involved. Less frequent, but not to be excluded, is infection induced by viral agents, such as Adenovirus and Poliomavirus BK.
All these infections affecting the urinary tract can originate for various reasons; in most cases these microorganisms come from the intestine, are eliminated with the faeces and migrate from the anal region towards the external opening of the urethra, and then rise up to it. to reach the bladder (in this regard, I remind you that the urethra is that small tube through which urine is expelled from the bladder towards the outside). Poor intimate hygiene, sexual intercourse and the use of urinary catheters can favor these infections, which are much more common in women than in men.
Non-infectious haemorrhagic cystitis, on the other hand, can occur above all as a complication of radiotherapy or treatments with immunosuppressive drugs, especially when they involve the use of cyclophosphamide and ifosfamide. Not only: haemorrhagic cystitis can be a consequence of already existing disorders, such as , for example, gynecological or prostate inflammation that can extend to the bladder.
In addition to sexual intercourse, especially if unprotected, and poor intimate hygiene, the risk factors for haemorrhagic cystitis can also include the use of too aggressive intimate cleansers, spermicidal creams or other irritants, constipation, diabetes , pregnancy, menopause, the use of tampons, invasive medical devices, such as the catheter, and mechanical contraceptives, such as the diaphragm.
As for the symptoms, we anticipated that these are similar to those of cystitis so to speak simple. The only difference is that in hemorrhagic cystitis the inflammation manifests itself in a more acute form; consequently, the symptoms present themselves in a more intense and marked way. For example, the pain when urinating is more intense, as is the burning sensation, which persists even after the urinary stream is over.
In addition to this, haematuria, ie the appearance of traces of blood in the urine, clearly stands out among the symptoms characterizing hemorrhagic cystitis. In this regard, doctors speak of macrohematuria when the urine visually changes color, taking on pink / purple or bright red tones based on the extent of blood loss; vice versa, when the haemorrhage is not visible to the naked eye we speak of microhematuria, a condition that is ascertained by examining the urinary sediment under a microscope.
As we have seen, hematuria can be accompanied by urinary irritative symptoms, such as urgency and increased frequency of urge to urinate. Other symptoms that may be encountered are pain in the lower abdomen and lumbar area, general malaise, fever and pain. during sexual intercourse.
In the presence of the symptoms of cystitis, it is necessary to quickly reach the diagnosis, in order to identify the causes of the inflammation and choose the most valid therapy. For this reason, usually, after having collected the relevant aspects of the disorder from the patient, the doctor proceeds with appropriate tests to ascertain the cause.
First of all, a complete urinalysis and urine culture must be performed to isolate any germ responsible for the inflammation.
If the presence of a bacterial agent is confirmed, an antibiogram is performed to identify the most effective antibiotic therapy to eradicate the specific bacterial infection.
Other specific tests such as cystoscopy, urography and ultrasound of the urinary tract are useful for evaluating lesions typical of hemorrhagic cystitis.
The therapy prescribed to counter the inflammatory process characteristic of hemorrhagic cystitis provides for several fronts of intervention, in relation to the causes of cystitis. Usually, in cases of infectious etiology, oral pharmacological therapy with antibiotics is combined with the use of urinary antiseptics and an adequate diet. Supportive therapy also includes the prescription of painkillers and antispasmodics, to reduce pain and inflammation. some cases can be instilled directly into the bladder of haemostatic, cytoprotective and antiseptic substances.The therapy can also last over time depending on the severity of the condition.
To assist in the treatment of bladder inflammation, it is suggested to increase the intake of fluids. Drinking a lot of water, in fact, hinders the ascent of bacteria along the urethra due to the washing action of the urine on the urinary tract; for the same reason, it dilutes the microbial load and favors its elimination with diuresis.
In the preventive field, as seen for non-haemorrhagic cystitis, it is possible to adopt simple precautions, which I will summarize briefly. First of all, it is recommended to urinate when you feel the need, thus avoiding holding urine for too long. Furthermore, it would be better to empty your bladder both before and after sexual intercourse.
Among other useful precautions, it is good to wear cotton underwear, avoiding the habitual use of clothing that is too tight and made of synthetic fabric. It is advisable to avoid occasional unprotected sexual intercourse, limit alcohol intake and fight constipation with a diet rich in vegetables and fruit and with plenty of water. The stagnation of feces in the colon, in fact, favors the proliferation of pathogenic germs, which then, as we have seen, can invade the urogenital system.
Lastly, daily intimate hygiene must not be neglected, while avoiding the use of too aggressive soaps or cosmetics. Therefore, only mild and slightly acidic intimate cleansers should be used.