With this video we will get to know more closely a very common disease that affects the thyroid gland, enlarging the waist, making you intolerant to the cold and always tired.
I'm talking about hypothyroidism, a disease in which the thyroid gland produces insufficient amounts of thyroid hormones. This deficit determines a generalized slowdown of metabolic processes and an imbalance of many bodily activities.
Trying to give a more precise and complete definition, hypothyroidism can be the consequence of defects related to the synthesis, accumulation, secretion, transport or peripheral action of thyroid hormones. All this causes their deficiency or in any case a reduction in their functions at the target cell level.
The first distinction between all these forms of hypothyroidism is that between primary hypothyroidism and secondary hypothyroidism.
Primary hypothyroidism is due to causes that directly affect the thyroid. In the case of primary hypothyroidism, the lack of thyroid hormone production therefore depends on alterations that directly affect the thyroid.
Secondary hypothyroidism, on the other hand, is due to a dysfunction of the pituitary gland, which controls the synthesis of thyroid hormones through the TSH hormone. Although it is very rare, remember that there is also a tertiary hypothyroidism, due to a malfunction of the hypothalamus ( which in turn controls the thyroid via the hormone TRH). In both cases, the insufficient secretion of the pituitary hormone TSH or the hypothalamic hormone TRH results in a reduced stimulus to the production of thyroid hormones. Consequently, the thyroid gland functions poorly and therefore hypothyroidism occurs.
Finally, there are rare forms of hypothyroidism caused by a generalized resistance of the cells to thyroid hormones. In practice, in these cases the thyroid hormones are present in normal quantities in the blood, but the cells become insensitive to their action. In similar circumstances, some receptor defects can cause the inefficiency of thyroid hormones at the peripheral level despite being present in adequate or even higher than normal quantities. This is a bit like what happens in the early stages of type 2 diabetes mellitus, when the cells develop resistance to the action of insulin causing hyperinsulinemia and, little by little, functional exhaustion of the beta cells of the pancreas responsible for the synthesis of insulin. .
Another important distinction must be made between acquired and congenital forms of hypothyroidism. Acquired hypothyroidism occurs when the thyroid decreases its activity later in childhood. Congenital hypothyroidism, on the other hand, is present from birth. and can be caused by a thyroid malformation or iodine deficiency during pregnancy.
When the thyroid is underdeveloped or absent, it produces insufficient thyroid hormones, triggering hypothyroidism. On other occasions, the gland grows normally but is unable to produce hormones from birth. Whatever the cause, the gland grows normally. 'congenital hypothyroidism is always a serious condition. We remember, in fact, that thyroid hormones are essential during fetal and neonatal development. Inadequate thyroid hormone production in a child can lead to problems in the development of the skeleton, but also deficiency of growth and mental retardation; if hypothyroidism is not treated promptly, it can therefore cause irreversible damage, especially to the central nervous system, leading to the so-called cretinism. For this reason, in the first week of life, all newborns are subjected to one screening that allows you to identify the disease.
As we have seen, hypothyroidism may depend on some disorders that directly involve the thyroid gland, or on insufficient production of the pituitary thyroid stimulating hormone (TSH).
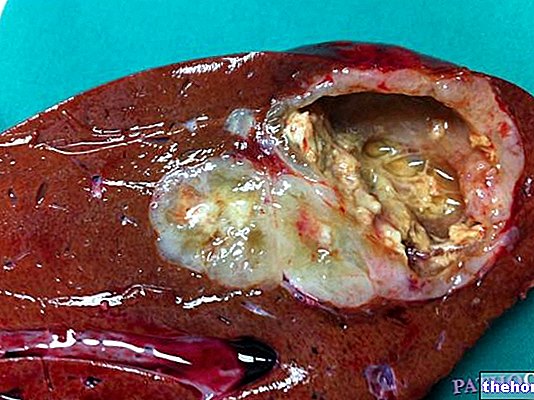
The most frequent cause of hypothyroidism is Hashimoto's thyroiditis, in which an autoimmune reaction causes the body to produce antibodies against thyrocytes, which are the thyroid cells. Over time, this process destroys thyroid cells, which consequently reduce their ability to produce hormones.
Another common cause of hypothyroidism is iodine deficiency. In this case, TSH stimulates the thyroid follicles to increase the endocrine activity of the thyroid gland and thus compensate for the reduced hormonal synthesis. However, if iodine is lacking, this attempt fails. An inadequate amount of iodine, mainly related to poor food intake, it can therefore favor the onset of goiter, which we remember is the increase in thyroid volume. In fact, the exaggerated stimulus of TSH ends up increasing the size of the gland, which unsuccessfully tries to produce more hormones by increasing its volume .
Hypothyroidism can also arise from iatrogenic causes, that is, as a side effect or complication of medical treatment. For example, hypothyroidism is very common after total or partial surgical removal of the thyroid gland, or after administration of radioactive iodine for the treatment of hyperthyroidism or certain thyroid cancers. In addition, iatrogenic hypothyroidism may represent the consequence of antithyroid therapy, such as methimazole, or drugs that can interfere with thyroid function, such as amiodarone, used for heart arrhythmias, and lithium, prescribed for certain psychiatric problems.
As mentioned, the symptoms of hypothyroidism vary considerably depending on the age of onset, the duration of the hormonal deficiency and its severity.
The reduced activity of the thyroid gland is expressed with the typical signs of a generalized slowdown of the metabolism. Common symptoms and signs are therefore tiredness, drowsiness, constipation, dryness and pallor of the skin, fragility and hair loss, and a feeling of cold due to the slowing of the basal metabolism. The brain also slows down its functions and memory and concentration problems occur, sometimes accompanied by depression. From a cardiological point of view, in the presence of hypothyroidism there is arterial hypotension and a reduction in the efficiency of the heart muscle. Menstrual irregularities appear in women of childbearing age, while men have erectile dysfunction. Other disorders related to hypothyroidism may include the increase in cholesterol levels, the increase in body weight and the appearance of goiter. Myxedema is also common, which consists of a characteristic swelling due to the accumulation of fluids in the subcutaneous tissues.
The presence of hypothyroidism can therefore be hypothesized on the basis of the symptoms reported by the patient and on the clinical signs that emerged during the medical examination.
The diagnosis is then confirmed with some blood tests. Blood tests assess whether the levels of thyroid hormones, TSH and anti-thyroid peroxidase antibodies are within normal limits.
In the case of hypothyroidism, the levels of thyroid hormones in the blood are typically below normal limits, but they can also be at normal levels. The TSH value, which I remind you to be the hormone produced by the pituitary that stimulates the thyroid, tends to be above the norm and this indicates a slowing down of the gland functions. In fact, to compensate for the reduced amount of thyroid hormones in circulation, the pituitary gland produces a greater amount of TSH.
As far as the dosage of the anti-thyroid peroxidase antibodies is concerned, this blood test allows to detect the possible presence of the antibodies responsible for the most common form of hypothyroidism, ie the autoimmune one (which as we have seen is called Hashimoto's thyroiditis).
Thyroid ultrasound, scintigraphy and fine needle aspiration are a useful complement for the evaluation of the clinical case, as they provide information on the morphology and functional capabilities of the thyroid.
The standard treatment of hypothyroidism is hormone replacement therapy. This treatment is based on the administration of drugs based on synthetic thyroid hormones, such as levothyroxine sodium.
The purpose of the treatment, in fact, is to bring the hormonal values back to normal and compensate for the metabolic imbalance. Compensation for reduced thyroid function is possible through the oral intake of the quantities of thyroid hormones that the body is unable to produce independently.
The therapy is therefore fundamentally pharmacological and, even if it must be followed throughout life, it manages to effectively keep hypothyroidism under control.