Before starting our journey, it is important to point out that early diagnosis is a formidable weapon to minimize the risks of serious prostate problems. This is true both for tumors and benign prostatic hyperplasia, and for the relative consequences on sexual life and on male fertility. In this regard, I remind you that prostate cancer is currently the most common cancer among men. In particular, they are men who are over 50 years of age to run the greatest risks, not only for prostate cancer, but also for prostatic hypertrophy. For this reason, after the age of 50, the execution of specific tests for investigating prostate health is strongly recommended, even in the absence of symptoms. Furthermore, in the presence of any prostate or genitourinary problem, in general, the good habit of contacting the urologist - who is the reference specialist for the urinary tract and the male genital system - should also be widespread in young adults Having made this necessary premise, let's see in detail which tests are useful for assessing the health of the prostate.
For a correct and early diagnosis of prostatic pathologies, the urologist can use various tests. Among these, the best known and sometimes feared are: the PSA dosage, digital-rectal exploration of the prostate, trans-rectal prostatic ultrasound and possibly prostate biopsy. Thanks to these tests it is often possible to diagnose prostate pathologies at an early stage, not yet complicated and therefore easily treatable. Just think of the importance of early diagnosis in the case of prostate cancer; in such circumstances, identifying the disease when it is still in its early stages almost always ensures complete recovery. Precisely for this reason, rectal exploration and PSA dosage represent cancer screening tests. In this regard, I would like to open a small parenthesis. I remind you that screening is a strategy that involves carrying out medical examinations on a specific population considered at risk, in order to identify a particular disease in its earliest stages. For example, as regards the female population, the Pap test is a screening method used to identify cervical cancer, while mammography it is indicated for diagnosing breast cancer. Specifically, the execution of the Pap test is recommended every three years starting from 25 years of age, while mammography is recommended for all women who have reached the age of 50 every 2 years. men than women for colon cancer; specifically, from 50 years of age it is normally suggested to search for occult blood in the stool once a year, which can be replaced by a sigmoidoscopy once every 5 years or by a colonoscopy every 10 years. Regarding prostate cancer, the validity of screening is still a matter of debate. In fact, alongside the indisputable benefits of early diagnosis, the risks of over-treatment must be considered, therefore the risk of treating prostate cancers that would not require treatment, since they are characterized by such a slow progression as not to affect the patient's survival. Such treatments are not only useless, but even counterproductive, as they increase public health costs and are a source of anxiety, worries and possible post-operative complications for the patient.
In any case, digital rectal examination of the prostate and the PSA dosage are often part of the routine urological examination and should always be performed in some categories of patients "at risk" for familiarity, urinary symptoms and ethnicity. To conclude, I want to clarify that screening is not synonymous with diagnosis; screening tests, in fact, have the purpose of identifying in a population considered at risk the individuals in which this risk is more consistent. screening simply indicates that it is advisable to undergo further medical investigations, which will then confirm or deny the presence of the disease.
The simplest, but also most discussed test to investigate prostate health is the blood dosage of the so-called prostate specific antigen, or more simply PSA. A simple blood sample allows you to measure its plasma levels. I remind you that PSA it is an enzyme produced by prostate cells with the purpose of keeping seminal fluid fluid. Even in normal conditions, a small amount of PSA is found in the blood. However, when these values exceed the threshold of 4 nanograms per ml of blood they represent an alarm bell for a possible prostate malfunction. In particular, elevated PSA levels or rising levels over time could indicate a number of conditions, including prostatitis (which is inflammation of the prostate), benign prostatic hypertrophy or cancer of the prostate. This is because diseased, inflamed, or cancerous glandular cells produce more PSA than normal cells. Currently, PSA is used as a "marker" for prostate cancer, but it is important to point out that the test is not accurate enough to rule out or confirm the presence of cancer. Just think that an ejaculation within 48 hours of the test can give rise to false positive results; in other words, it generates PSA increases that are not dependent on a real prostate disorder. For this reason, the PSA test must always be interpreted in the context of the patient's clinical picture and must be associated with and complemented by rectal examination. Let us now see what this last examination consists of.
Rectal examination is the simplest, most immediate and perhaps feared diagnostic procedure to check the condition of the prostate. In fact, it represents an indispensable assessment for the study of any prostatic pathology. The rectal examination allows to identify, to the touch, any alterations of the gland. During the urological examination, the doctor - protected by a lubricated latex glove - gently introduces a finger into the patient's rectum. In this way he can palpate the posterior surface of the prostate gland and the surrounding tissues to evaluate the increase in volume, the consistency and the possible presence of suspicious nodules. To the touch, healthy prostate tissue is smooth and smooth. For comparison, it has almost the texture of fabric where the thumb joins the palm of the hand. Conversely, the tumor tissue is solid, hard and irregular on palpation. Unfortunately, rectal examination does not always succeed in demonstrating the presence of prostate cancer; as PSA cannot therefore be used to establish a certain diagnosis. Therefore, if the search for PSA and rectal exploration reveal the suspicion of cancer, we proceed with targeted investigations to formulate a safe diagnosis.
The first of these investigations is represented by trans-rectal ultrasound. It is a simple examination performed by introducing an ultrasound transducer into the patient's rectum, to obtain a detailed study of the prostatic morphology. The trans-rectal ultrasound is able to document the increase in volume of the gland, to define its margins, to highlight the signs of both acute and chronic inflammation and to locate any suspicious areas for prostatic neoplasia.
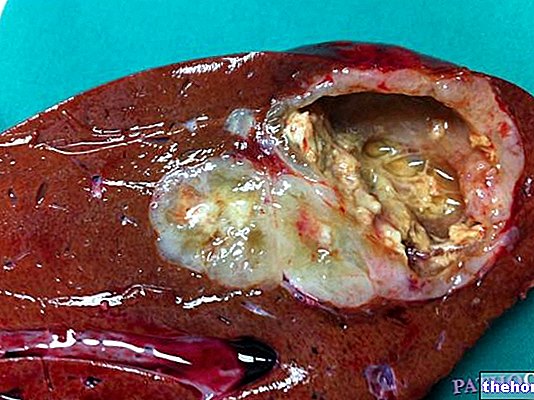
The only test capable of defining the diagnosis of cancer with certainty is the prostate biopsy. This examination can be performed trans-rectally or trans-perineally, that is, through the region between the rectum and the scrotum. The method, performed under local anesthesia and under ultrasound guidance, involves the insertion of a fine needle into the prostate. In this way the doctor can take a variable number of samples, approximately 10-12, coming from different areas of the gland and especially from any suspicious areas. The samples collected in this way are then subjected to histological examination under a microscope to ascertain the presence of neoplastic cells. In this way, the biopsy confirms the presence of prostate cancer and allows to determine the type, position and " stage "of the neoplasm, ie its severity and extent.
If cancer cells are detected during the examination of the prostate sample and there is a significant likelihood that the cancer has spread from the prostate to other parts of the body, further tests may be recommended. The doctor, in particular, should proceed to evaluate the cancer. malignancy index, that is, to establish how much the tumor cells are altered compared to those of normal tissue. The more the cancer cells differ from normal cells, the more aggressive the tumor will be. To quantify this data, which is indispensable for establishing adequate therapeutic strategies, the Gleason classification system is used, named after the American pathologist who defined it. To establish the extent of the tumor, therefore to define the staging, other tests may be necessary such as ultrasound, Computed Tomography (CT), Nuclear Magnetic Resonance and bone scintigraphy These investigations evaluate qu anto the tumor is widespread and if it involves nearby lymph nodes, surrounding tissues or other organs even distant from the prostate.