Over the years, the repetition of the typical manifestations of Ménière's syndrome leads to a worsening of the patient's general state of health. For example, the hearing loss can be permanent, even reaching complete deafness.
Currently, the precise cause of Ménière's syndrome is not known; the only certain fact is that the disease is characterized by an abnormal accumulation of endolymph inside the so-called labyrinth of the inner ear.
Unfortunately, there is no specific cure for Ménière's syndrome; however, patients can count on various symptomatic treatments, capable of appreciably improving the standard of living.
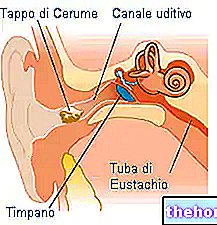
Inner Ear and Cochlea: a brief review

The inner ear essentially consists of the membranous labyrinth (or simply labyrinth).
The labyrinth of the inner ear comprises two hollow structures: the cochlea, which is the organ of hearing, and the vestibular system (or vestibular apparatus), which is the organ of balance.
Each of these organs is connected to the brain by means of a nerve: the cochlea via the cochlear nerve, while the vestibular system via the vestibular nerve.
A fluid, called endolymph, circulates inside the cochlea and the vestibular system.
Rich in potassium, endolymph is essential for auditory perception and balance, as it plays a decisive role in the transmission of nerve signals / impulses from the inner ear to the brain.
This relaxation process is responsible for:
- Damage to the cells that make up the labyrinth and cochlea epithelium;
- The increase in internal pressure;
- The alteration of nerve signaling between the inner ear and the brain.
To corroborate the thesis according to which it is precisely the hydrops that trigger the Ménière syndrome are at least a couple of important observations:
- The accumulation of endolymph is an episodic and transitory phenomenon, at the end of which the normal auditory perception and balance is re-established; for example, when the blood pressure returns to normal, the patient no longer feels symptoms.
- The succession of endolymph accumulations inside the labyrinth and cochlea, over the years, gradually worsens the auditory perception, to the point of irreparably damaging it.
At this point, it is legitimate to ask what are the factors that induce hydrops.
Ménière's Syndrome: What are the Causes?
Currently, the precise cause of Ménière's syndrome is unknown. However, there are several theories about it; over time, in fact, experts have hypothesized that the problem may be the consequence of:
- Vascular abnormalities similar to those that cause migraines;
- Viral infections;
- Allergies;
- Autoimmune mechanisms. To support this theory is the common association between Ménière's syndrome and autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus or psoriasis;
- Genetic factors and familiarity;
- Process of partial ossification of the canals of the vestibular apparatus. The supporters of this hypothesis believe that ossification causes a deformation of the membranous labyrinth such as to cause the accumulation, in some sites, of the endolymph;
- Alterations of the ionic / saline content of the endolymph. For a correct nerve signaling between the inner ear and the brain, a certain balance of salts and ions inside the endolymph is fundamental.
Did you know that ...
Not all people with endolymphatic hydrops develop Ménière's syndrome; this evidence is one of the main reasons why it is difficult to understand the exact cause of the disease.
, which cause a lack of balance;Less common symptoms are nystagmus and sudden fainting without loss of consciousness.
Symptoms of Ménière's Syndrome: the Initial Phase
In an early stage of the disease, the typical symptoms of Ménière's syndrome manifest themselves as transient and episodic attacks, the duration of which can vary from 20 minutes to a few hours.
3-4 in number per day, these episodes usually begin sharply and suddenly, and affect only one ear.
It is very common that, for a few consecutive days or even for a week, the patient is subject to attacks that are close in time.
Once these manifestations are over, a period of remission follows, interrupted by another series of attacks.
On average, an individual with early Ménière syndrome experiences 6 to 11 such "crises" in a year.
Dizziness can occur without being accompanied by hearing loss, while nystagmus, when it appears, is usually short-lived.
However, the reverse can also occur; therefore, it is difficult to accurately establish the symptoms, as the latter varies from patient to patient.
Symptoms of Ménière's Syndrome: the Advanced Phase
When Ménière's syndrome is at an advanced stage, some symptoms begin to take on a permanent character. This is the case, for example, with hearing loss; in fact, a patient subject to repeated attacks over the years develops irreversible damage to the structures that make up the labyrinth and the cochlea.
The evolution, in some cases, is so severe that it can lead to complete deafness of the affected ear.
Although less common, the sensation of "ringing" in the ear (tinnitus) can also become a lifelong symptom.
The same is also true for lack of balance and dizziness.
The following table summarizes the characteristics of the main symptoms of Ménière's syndrome, in its early and advanced stages.
For further information: Symptoms of Ménière's SyndromeMénière syndrome: absence of signs
Premise: in medicine, an objective finding is considered a sign, recognized by the doctor in a patient; the symptom, on the other hand, is a subjective sensation reported by the patient, such as dizziness.
Ménière's syndrome has no distinctive diagnostic signs. This complicates the diagnosis, as will be seen later.
Ménière's Syndrome: Complications
The main complications of Ménière's syndrome are those, already mentioned in part, of the advanced stage of the disease:
- Complete deafness of the affected ear;
- Involvement of the healthy ear, after 2-3 years;
- Depression and anxiety, due to poor quality of life, cause repeated bouts of nausea and vomiting.
Their necessity depends on the fact that the disease is characterized only by non-specific symptoms (hypoacusis, tinnitus, vertigo, etc.), which also arise in other pathological circumstances; therefore, a simple audiometric test, for example, is not sufficient to confirm suspicions.
Ménière's Syndrome: Differential Diagnosis
A detailed differential diagnosis is of great help in ruling out pathologies similar to Ménière's syndrome or that cause the same symptoms.
The main investigations are aimed at excluding conditions such as: acoustic neuroma, transient ischemic attack (TIA), anomalies of the arteries of the labyrinth, the toxic effects of some drugs on the vestibular system, migraine, cervical spondylosis or some systemic diseases (anemia, syphilis, etc.).
These morbid circumstances, very often, cause only one of the typical symptoms of Ménière's syndrome.
The tests useful for the differential diagnosis are different; among these, the most practiced are:
- Blood tests;
- Nuclear magnetic resonance;
- Electrocochleography.
The following table summarizes the pathological conditions that can be confused for Ménière's syndrome.
Differential diagnosis
- Anemia;
- Diabetes mellitus;
- Hypothyroidism;
- Autoimmune diseases;
- Syphilis.
Ménière's Syndrome: Analysis of Clinical Symptoms
There are some diagnostic criteria regarding vertigo and tinnitus; here's what they are:
- The feeling of vertigo must last at least 20 minutes and must not be a sporadic and isolated episode. In other words, it must be followed by at least one "more dizzying crisis. Only in this case, it is a typical attack of Ménière's syndrome.
Furthermore, the Romberg test is useful in assessing the patient's coordination and balance. - Tinnitus, on the other hand, must be associated with the so-called "closed ear", or fullness headset.
Ménière's Syndrome: Audiometric Tests
Finally, audiometric tests are used to assess the real hearing capacity of the patient, who complains of partial or complete deafness. The tests put in place are the Rinne test and the Weber test.
regular and a low-salt diet can have a significant impact on the symptomatological picture.Ménière's syndrome: drugs
Medicines for the Treatment of Vertigo and Nausea
For the management of dizziness, nausea and vomiting, antiemetic, prokinetic and antivertigenic drugs are used; in particular, we note:
- Prochlorperazine (antiemetic);
- Domperidone (prokinetic);
- Metoclopramide (prokinetic);
- Cinnarizine (antivertiginous).
These medicines available in various formulations: suppository, tablet or for parenteral use.
Medicines to Prevent Vertigo and Nausea
To prevent attacks of vertigo and nausea, medications such as:
- Betahistine. It has a positive effect in reducing the number and severity of dizziness and nausea.
- Gentamicin. Administered by transtympanic injection, this medicine acts on the nerve signal that regulates balance.
The use of gentamicin is reserved only for cases in which the other drugs have proved to be ineffective. - Diuretics and beta-blockers. They serve to decrease the pressure inside the vestibular apparatus, pressure which is high due to the accumulation of endolymph.
It should be noted that the actual efficacy of these drugs is the subject of conflicting opinions.
Ménière's Syndrome: Surgery
When pharmacological treatments for the management of Ménière's syndrome do not produce the desired results, the conditions exist for resorting to surgery.
There are four main surgical options:
- Labyrinthectomy: is the removal of the labyrinth of the inner ear affected by the disease.
- Decompression of the endolymphatic sac: it aims to reduce the pressure of the endolymph inside the labyrinth.
- Section of the vestibular nerve: involves the incision of the balance nerve, with the aim of interrupting the abnormal signaling between the inner ear and the brain.
- Micropressure therapy: it is based on the use of a special instrument, which sends pressure impulses capable of making the endolymph drain from the site where it has accumulated.
The ultimate goal is to lower the too high pressure inside the labyrinth.
The first three surgeries are highly invasive, while the last (micropressure therapy) is only moderately invasive.
Ménière's Syndrome: Hearing Aids, Sound Therapy and Physiotherapy
For hearing loss (permanent or transient), the use of hearing aids may be useful; these devices serve to increase the patient's ability to perceive sounds.
For tinnitus, the "whistling" in the ear, experts recommend sound therapy; this treatment consists in distracting and relaxing the patient by listening to music.
Sound therapy seems to be able to relieve the sensation of tinnitus with some success.
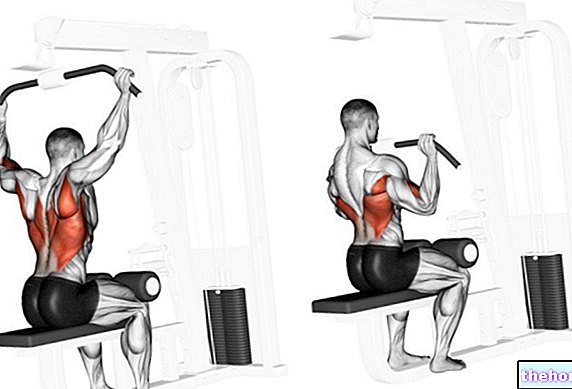
To improve balance and coordination skills, physiotherapy is indicated.
Did you know that ...
There are also specific medications for the treatment of ringing in the ears.
Ménière Syndrome and Lifestyle
As partly anticipated, a healthy lifestyle helps prevent and improve the symptoms of Ménière's syndrome.
In this regard, the main recommendations are:
- Low-sodium diet, to keep the pressure of body fluids low, including endolymph;
- Not smoking;
- Don't abuse alcohol and caffeine;
- Regular physical exercise, to distract the patient and keep him active (those prone to dizziness and nausea tend to lie down and not perform motor activities).