Generality
Mitral valve prolapse (PVM), or mitral valve prolapse, consists of an incorrect movement, at the time of closure, of the flaps (or cusps) that make up the mitral valve of the heart.
Placed to control the blood flow between the left atrium and ventricle, the mitral valve, if not properly closed at the time of systole, causes blood regurgitation in the direction of the left ventricle → left atrium. For this reason, mitral valve prolapse is one of the causes of mitral regurgitation. The anomalous positioning of the cusps is caused by a degeneration of the tissue of the cusps themselves or by the rupture of one of the structural elements of the mitral valve.

What is mitral valve prolapse
Mitral valve prolapse (PVM), or mitral valve prolapse, consists of an abnormal closing movement of the cusps (or flaps) that make up the mitral (or mitral) valve of the heart. Under normal conditions, the mitral valve controls blood flow in the left atrium - left ventricle direction and prevents reflux in the opposite direction during ventricular systole thanks to a hermetic closure. On the appearance of a prolapse of the mitral valve, however, during the contraction phase of the ventricle (ventricular systole), a portion of blood, instead of entering the aorta, goes back and goes back to the left atrium; this happens because the valve orifice is not completely closed. This is the so-called regurgitation of blood, which characterizes another important heart disease: mitral insufficiency; it will be seen, later on, that the two valve defects, prolapse and mitral insufficiency, they are closely connected.
Mitral valve prolapse affects women more than men. It is also more frequent in long-limbed subjects, with elongated and flattened thorax, as well as in individuals suffering from dorsal scoliosis.
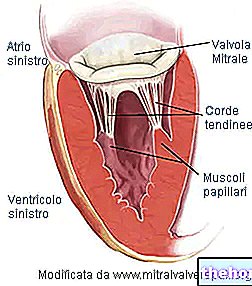
Before proceeding with the description of the main causes that determine a mitral valve prolapse, it is good to recall some fundamental characteristics of the mitral valve. Recalls that will also be useful to describe the appearance and functioning of the same valve when it is subject to prolapse, that is, respectively, the pathological anatomy and pathophysiology.
Therefore:
- The valve ring. Circumferential structure of connective tissue that delimits the valve orifice.
- The valve orifice measures 30 mm in diameter and has a surface area of 4 cm2.
- Two flaps, front and back. For this reason, the mitral valve is said to be bicuspid. Both flaps enter the valve ring and face the ventricular cavity. The anterior flap faces the aortic orifice; the posterior flap, on the other hand, faces the wall of the left ventricle. The flaps are composed of connective tissue, rich in elastic fibers and collagen. To facilitate the closure of the orifice, the edges of the flaps possess particular anatomical structures, called commissures. There are no direct controls, of a nervous or muscular type, on the flaps. Likewise, there is no vascularization.
- The papillary muscles. There are two of them and they are extensions of the ventricular muscles. They are supplied by the coronary arteries and give stability to the tendon cords.
-
The tendon cords. They serve to join the valve flaps with the papillary muscles. As the rods of an umbrella prevent it from turning outward in strong winds, the tendon cords prevent the valve from being pushed into the atrium during ventricular systole.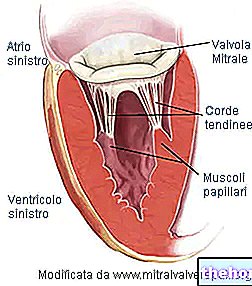
Causes of mitral valve prolapse.
Pathological anatomy and pathophysiology
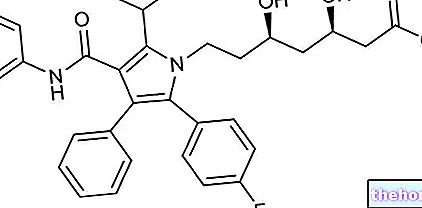
The main cause of mitral valve prolapse is degeneration of the loose connective tissue that constitutes the flaps (or cusps) of the mitral valve. It is a myxomatous degeneration, as the intermediate layer of the connective tissue of the valve flaps is subject to myxoma. Myxoma is a particular neoplastic form (tumor), when the extracellular matrix that makes up the cardiac connective tissues is altered; therefore, the matrix varies in composition and we have that:
- Collagen fibers are produced inadequately.
- The mucopolysaccharides of the basic substance increase in quantity.
Myxomatous degeneration takes place in some components of the mitral valve and changes its morphology:
- The valve flaps become more elongated, yielding and thickened.
- The tendon cords stretch and, sometimes, can even break.
- The valve ring increases its circumference.
Altered in structure, the cusps no longer seal the valve orifice.
Failure to close the valve is usually attributable to only one of the flaps, the rear one. Sometimes, however, both are affected. The anomaly, in the closing movement, consists in a flexion of the flaps towards the atrial cavity. In other words, if in normal conditions, the flaps turn towards the ventricle, in cases of prolapse, they curve on the opposite side, towards the cavity of the left atrium. The term prolapse, in fact, means the escape of a bowel from the cavity in which it is contained through a "natural opening. The definition resembles that of a" hernia. In the specific case, we are not talking about a real hernia, since the bowel in question is a flap of the valve, but the behavior is very similar.
The alteration of the normal closure of the mitral valve, during systole, causes the same pathophysiological adaptations that characterize mitral insufficiency. Therefore:
- The regurgitation of blood flows into the left atrium and enlarges its size. The cardiac output is depleted of the regurgitation rate. Therefore, the blood circulation is inefficient. The individual copes with this situation by increasing the respiratory acts.
- At the next diastole, the mitral valve opens, causing regurgitation to flow from the atrium to the left ventricle. This is a situation that usually does not happen and that affects the pressure gradient between the atrium and the ventricle.
- Regurgitation, inside the ventricle, raises the ventricular pressure, altering the normal balance with the atrial pressure value. A situation called left ventricular decompensation is determined.
These three effects on blood flow are not always equally critical. In other words, mild forms of mitral valve prolapse determine a "mild mitral insufficiency. The same can be said of moderate forms, while the case in which a" other heart disease is associated with mitral prolapse is quite different: the consequences , on blood flow, are more serious.
Although less frequent, there are other causes that cause mitral valve prolapse.
- Marfan syndrome
- Ehlers-Danlos syndrome
- Rheumatic endocarditis
- Ischemic heart disease
- Trauma
- Obstructive hypertrophic cardiomyopathy
- Surgery on the mitral valve
- Lupus erythematosus
- Duchenne muscular dystrophy
- Atrial septal defect
- Hyperthyroidism
- Turner syndrome
- Ebstein's disease
These include Marfan syndrome and Ehlers-Danlos syndrome. They are two congenital pathologies, that is, present from birth. They cause alterations in the connective tissues that follow the structural and morphological changes induced by the myxomatous degeneration described above.
Symptoms and signs
Mitral valve prolapse presents with symptoms very similar to that of mitral insufficiency. However, it is fair to point out that, in most cases, mitral prolapse is asymptomatic, that is, it does not present symptoms. In this case, the individual bearer of this anomaly carries out a normal life, can play sports and carry out any other physical activity of a healthy person.
The most frequent symptoms are:
- Heartbeat
- Dyspnea from exertion
- Asthenia
- Chest pain
- Vertigo
- Syncope
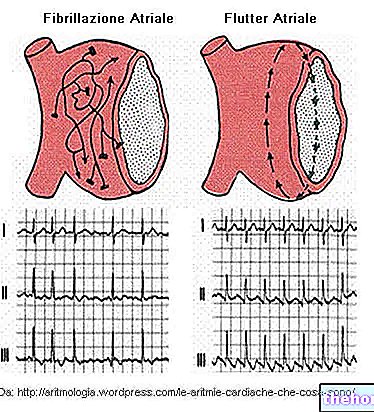
Heartbeat, also known as palpitation, is the most common symptom in those who experience mitral valve prolapse. Heartbeat consists of an increase in the intensity and frequency of the heartbeat; it usually manifests itself with a tachycardia, that is an increase in the speed of the heartbeat, but can sometimes give rise to different types of arrhythmias. Arrhythmias are changes in the normal heart rhythm. Heart rhythm that originates from a natural pacemaker, known as a sinoatrial node. Among the moderate and severe arrhythmias, ventricular extrasystole and atrial fibrillation are reported respectively.
Ventricular extrasystole consists in a contraction of the heart that occurs in advance of the regular heart rhythm, altering the succession of beats. It can be an isolated or repeated phenomenon: if repeated, the extrasystole is much more dangerous. Furthermore, isolated extrasystole is much more frequent, in terms of onset, than repeated extrasystole and atrial fibrillation.
Atrial fibrillation is a "cardiac arrhythmia, that is, an alteration of the normal heartbeat rhythm." It is due to a disorder of the nerve impulse coming from the sinoatrial node. It results in fragmentary and hemodynamically ineffective atrial contractions (that is, what concerns the blood flow). In the case of a mitral valve prolapse, the regurgitation of blood in the atrium reduces the blood volume pushed into the aorta by the ventricular contraction. In light of this, the organism's demands for oxygen are no longer satisfied. Faced with this situation, the individual affected by atrial fibrillation increases respiration , manifests palpitation, pulse irregularities and, in some cases, fainting due to lack of air. The picture can further degenerate: a continuously increasing regurgitation and the accumulation of blood in the vascular systems upstream of the left atrium, if associated with a "impaired coagulation, give rise to the formation of thrombi (solid, non-motile masses composed of platelets) inside the vessels. The thrombi can break down and release par ticellae, called emboli, which, traveling in the vascular system, can reach the brain, or the heart. In these locations, they become an obstacle to the normal circulation and oxygenation of brain or cardiac tissues, causing the so-called ischemic stroke (cerebral or cardiac). In the case of the heart, it is also referred to as a heart attack. In people with mitral valve prolapse, however, it is a rare event.
Exercise dyspnea is difficulty breathing. In the specific case, it arises from the decreased cardiac output of the left ventricle, due to the amount of blood regurgitated towards the left atrium. Therefore, the response of the organism consists in "increasing the number of respiratory acts, in order to counterbalance the volume. of range.
Similarly, syncope is another natural consequence of compromised outflow of blood from the left ventricle to the brain. In fact, syncope occurs when blood flow to brain tissue is reduced. The lower cardiac output, associated with mitral prolapse, prevents normal blood circulation of the brain tissue and this condition can occur both during exertion, or physical activity, and, if serious, at rest. Resting syncope is often associated with left ventricular malfunction and can cause sudden death. In those suffering from mitral valve prolapse, this is a rare event; on the other hand, the sensation of dizziness is much more common, also linked to the lower oxygenation of the brain.
Chest pain due to angina pectoris is a rare event. Angina pectoris, in this case, is due to "left ventricular hypertrophy, ie of the left ventricle, and not to a" occlusion of the coronary vessels. In fact, the hypertrophic myocardium needs more oxygen, but this request is not adequately supported by the "coronary implant, which remains unchanged. Therefore, there is an imbalance between the consumption and the supply of oxygen to the tissues. The pain typical of angina pectoris is felt in the left hemithorax.
Fatigue is a sense of weakness and lack of energy.
The characteristic clinical signs of a mitral valve prolapse are two:
- The click. It is a noise caused by the modified tendon cords.
- The systolic murmur. It originates from the regurgitation of blood through the defective valve during ventricular systolic contraction.
Both reveal themselves with listening.
Diagnosis
Mitral regurgitation can be detected by the following diagnostic tests:
- Stethoscopy.
- Electrocardiogram (ECG).
- Echocardiography.
Stethoscopy. The detection of a systolic murmur is one of the most important clues to diagnosing a mitral valve prolapse. The murmur is produced when the regurgitation of blood passes from the left ventricle to the left atrium. It is perceived in the systolic phase, since it is at this moment that the mitral valve is not closed as it should. The detection zone is in the 5th intercostal space, that is, the one coinciding with the position of the mitral valve. The other important diagnostic sign, the click, varies in intensity according to the positions taken by the individual who presents it.
ECG. By measuring the electrical activity of a heart with mitral valve prolapse, the ECG shows the wide variety of arrhythmias that can occur in a patient. The list is drawn up on the basis of the characteristics of frequency and danger: it starts with the most frequent and least dangerous and ends with the least frequent but most dangerous.
- Isolated ventricular extrasystoles.
- Tachycardia.
- Atrial fibrillation.
- Repeated ventricular extrasystoles
Diagnosis by ECG gives an idea of the degree of severity of mitral valve prolapse: if the outcome is comparable to that of a healthy individual, it means that it is not a severe form; conversely, the examination shows the irregularities mentioned.
Echocardiography. Using the ultrasound emission, this diagnostic tool shows, in a non-invasive way, the fundamental elements of the heart: atria, ventricles, valves and surrounding structures. From echocardiography, the doctor can detect:
- Abnormal behavior of the valve flaps and tendon cords.
- Anomalies of the left ventricle, during the phases of systole and diastole.
- Increased size of the left atrium (dilated atrium).
- The maximum flow rate and turbulent systolic flow of regurgitation, using continuous and pulsed Doppler techniques, respectively. From the first measurement, the pressure gradient between the left atrium and the left ventricle can be obtained; from the second, the extent of the regurgitation.
Therapy
The medical treatment of mitral valve prolapse, from less severe and asymptomatic to severe cases, is very similar to that of mitral insufficiency. The therapeutic approach therefore varies according to the severity of the heart disease. The asymptomatic forms, but also the mild ones, require preventive measures, aimed at avoiding bacterial infections, such as endocarditis, which affect the heart cavities. Periodic checks are also recommended every 2-3 years, but the individual, with a mild form of prolapse, can carry out any activity, including sports. The most used drugs, in mild forms of mitral valve prolapse, are:
- Beta-blockers and anxiolytics. They are used when mild arrhythmias occur.
The first appearance of symptoms and moderate / severe forms require more attention: in addition to drug therapy, surgery can become decisive.
The critical situations, which recommend the intervention, are:
- The ascertained rupture of the valve tendon cords.
- Repeated and gradually more severe arrhythmias.
- Increased atrial cavity ascertained following regurgitation
- Left ventricular failure.
These clinical findings are comparable to those that occur during a "moderate / severe chronic mitral insufficiency.
There are two possible surgical operations:
- Replacing the valve with a prosthesis. It is the most used intervention for the valves of those individuals, not young, with serious anatomical anomalies. A thoracotomy is performed and the patient is placed in extracorporeal circulation (CEC). The extracorporeal circulation is implemented through a biomedical device which consists in creating a cardio-pulmonary pathway replacing the natural one. In this way, the patient is guaranteed an artificial and temporary blood circulation that allows surgeons to interrupt the flow of blood in the heart, diverting it to another equally effective path; at the same time, it allows to operate freely on the valve apparatus. Prostheses can be mechanical or biological. Mechanical prostheses require, in parallel, an anticoagulant drug therapy. Biological implants last 10-15 years.
- Mitral valve repair. It is the most suitable approach for mitral insufficiencies of "non-rheumatic" origin. In other words, those caused by a mitral valve prolapse. The valve structures of the ring, cusps and / or tendon cords are compromised.The surgeon acts differently, based on where the valve lesion resides. Again, patients are placed in extracorporeal circulation. It is an advantageous technique, as the prostheses have some drawbacks: the biological ones must be replaced after about 10-15 years; the mechanical ones require the continuous administration, in parallel, of anticoagulants.