Generality
Atrial flutter is an "alteration of the heart rhythm that is located in the" atrium; as a result of this arrhythmia, the heartbeat becomes irregular and, usually, at a high frequency (tachycardia). Compared to atrial fibrillation, these changes in the beat are less marked and have a different impact on the ventricle.
Given the modalities of onset, two types of atrial flutter can be distinguished: a paroxysmal form, with abrupt and sudden onset, and a permanent form, with more gradual onset. In terms of causes, symptoms, diagnosis and therapy, the characteristics of atrial flutter and atrial fibrillation are very similar. In fact, as with atrial fibrillation, the onset may be due to pathological causes, such as heart disease or hyperthyroidism, or to other factors, such as alcohol and drug abuse, smoking, caffeine, etc. Possible also spontaneous onset in people with otherwise healthy hearts. As for the symptoms, the subject affected by atrial flutter presents palpitation, dyspnea, syncope, chest pain and asthenia, even if at times these disturbances are very mild or even absent.

Sometimes, atrial flutter and atrial fibrillation can occur in the same patient: these are circumstances that deserve considerable attention from the doctor, as they are usually linked to the formation of thrombi or emboli.
N.B .: to understand some concepts illustrated in the article, it is necessary to know the basics of anatomy and physiology of the heart illustrated in the general article on cardiac arrhythmias.
So is atrial flutter
Atrial flutter is an "alteration of the heart rhythm that originates in" the atrium and is characterized by:
- Frequent contractions.
- Irregular heartbeat.
- Sudden onset.
The arrhythmic disorder arises in the atrium and is transmitted to the ventricle. Therefore, cardiac output and blood circulation are also compromised. They both become irregular.
Atrial flutter afflicts about 1% of the population of Western countries; it occurs more in males and its incidence increases with age: the people most affected, in fact, are the sixties and over sixties.
Given the "area of onset", atrial flutter is classified among the supraventricular ectopic arrhythmias.
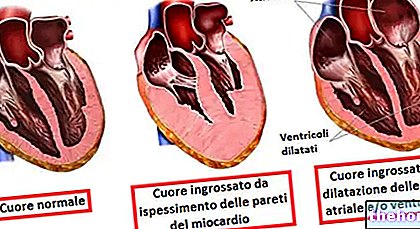
Compared to atrial fibrillation, the rhythm changes are less marked. In fact, if during an atrial fibrillation the atrial heart rate can reach 400 beats per minute, during an atrial flutter the atrial heart rate can rise to a maximum of 240-300 beats per minute. A lower frequency results in fewer contraction pulses. Therefore, what changes compared to atrial fibrillation is also the greater time given to the heart muscle (the myocardium) to "recharge" and become receptive to a new stimulus (refractory time). This time frame allows the heartbeat to be less messy.
Another important difference between flutter and fibrillation is the impact they have on the ventricle. During these two arrhythmic forms, part of the impulses are blocked at the level of the atrioventricular node, which stops part of the impulses directed towards the ventricle. This block is much greater in atrial flutter, so much so that the ventricular contraction can be as much as ¼ of the atrial one. The doctor, in fact, defines the flutter with the terms of 2: 1, 3: 1 or 4: 1, to indicate that a stimulus can pass through the atrioventricular block, respectively, every 2, every 3 or every 4. The consequences of atrioventricular block relate to cardiac output, which will be more or less affected according to the number of stimuli reaching the ventricle. It may seem complicated to understand this detail, but it is very important from a symptomatic point of view: in fact, the higher the ventricular rate, the more evident the symptoms. In other words, the ventricular rate can vary greatly, from 180 beats per minute to less than 100. The fact that the ventricular rate can fall within the normal range is not surprising: it often happens that flutter goes unnoticed for this very reason. .
Based on the impact on the ventricle and how it occurs, atrial flutter is divided into two forms:
- Paroxysmal. The heartbeat frequency is very high. The onset is abrupt and the atrial contractions overcome the atriventricular block with considerable effectiveness, by 2: 1 and, in some rare cases, even by 1: 1. The ventricular rate, therefore, can reach even 120-180 beats per minute The paroxysmal form characterizes the isolated manifestations, which occur in a healthy individual. It lasts a few hours, at most a few days, very often it ends on its own. This excludes the use of drugs or other therapeutic interventions.
- Permanent. The frequency is lower than in the paroxysmal form. The onset is less sudden, but more subtle, and the contractions overcome the atrioventricular node block with an "efficiency of 3: 1, 4: 1 and even 5: 1. Hence, the ventricular rate is lower than in the paroxysmal form and in some cases, it may not exceed 100 beats per minute. The permanent form can last for years and go unnoticed, despite being synonymous, in most cases, with an associated pathology. Specific therapy and general therapy are needed: the first to act against the associated pathology; the second to act against flutter.
Otherwise, it will be seen that flutter and atrial fibrillation have many characteristics in common.
Causes
The causes of atrial flutter are numerous. As with atrial fibrillation, the most often determining factors are heart disease. In fact, an individual with heart failure due to rheumatic or valvular heart disease is more prone to develop episodes of atrial flutter.
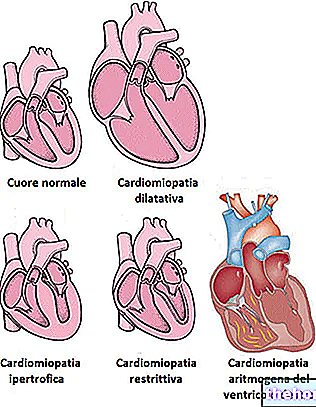
The most influential heart disorders are:
- Rheumatic heart disease.
- Valvular heart disease (or valvulopathy).
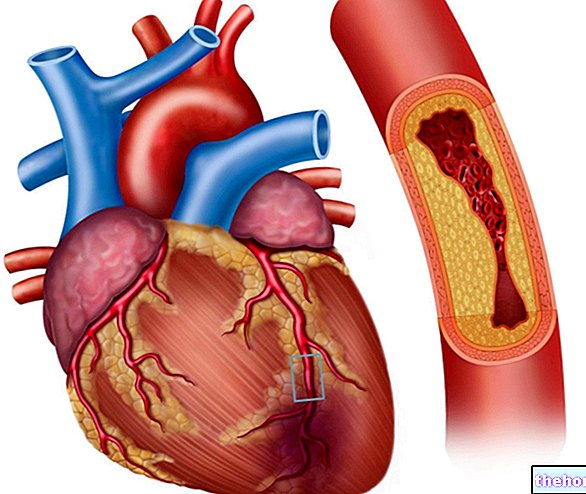
- Myocardial infarction.
- Coronary heart disease.
- Pericarditis.
- Hypertension.
Hypertension is not really a heart disease, but it is a predisposing factor to myocardial infarction and coronary heart disease.For this reason, it appears in the list.
Non-cardiac disorders, which cause flutter, are, on the other hand:
- Hyperthyroidism.
- Obesity.
- Gastroesophageal reflux.
- Respiratory diseases.
- Electrolyte imbalances.
Finally, some non-pathological factors can also determine the onset of atrial flutter. The arrhythmic episode usually appears, under these circumstances, in healthy individuals and has spontaneous exhaustion.
- Alcohol abuse.
- Drug abuse.
- Smoke.
- Anxiety.
- Medicines.
- Excess of caffeine.
Correcting these behaviors, not in line with a healthy lifestyle, helps solve the problem and prevent stable forms of atrial flutter. In fact, it should not be forgotten that some of the behaviors on the list are the prelude to the aforementioned heart diseases.
Symptoms and complications
The main symptoms are:
- Palpitation (or heartbeat).
- Vertigo.
- Syncope.
- Chest pain (angina pectoris).
- Dyspnea.
- Anxiety.
- Asthenia (weakness).
The symptoms are closely related to the form of atrial flutter experienced by an individual. The paroxysmal forms, at very high frequency, manifest more evident symptoms, but it should not be overlooked that the greatest danger lies behind the permanent forms. In fact, it is at the origin of these that there is a pathological disorder.
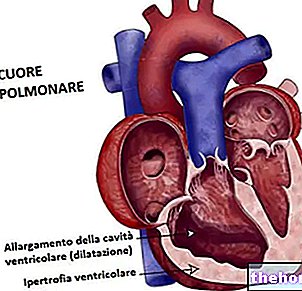
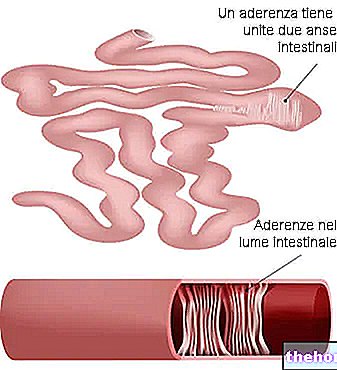
The most serious complication, induced by atrial flutter (albeit to a lesser extent than atrial fibrillation), is the predisposition, in the affected subject, to develop a cerebral ischemic stroke. This is due to the fact that the numerous irregular contractions, which affect first the atrium and then the ventricle, negatively affect cardiac output and blood flow. The latter becomes more turbulent. A turbulent flow has a high probability of creating lesions inside the vessels and consequently forming thrombi, ie solid and stable masses of platelets (thrombocytes), which serve to repair the lesion. The thrombus obstructs the blood flow, occluding the vessels. Due to the continuous passage of blood, it can flake and give life to emboli, that is free particles made of platelet cells. The emboli, traveling through the vascular system, can reach the brain and prevent the regular blood supply of the cerebral area. This complication is more likely to occur if, in the affected individual, episodes of atrial fibrillation alternate with atrial flutter or if the patient is affected by valve pathologies with atrial dilation (such as mitral stenosis).
The thrombo-embolic risk associated with atrial flutter is however lower than that of atrial fibrillation.
Diagnosis
An accurate diagnosis requires a cardiological visit. Traditional tests, valid for the evaluation of any atrial arrhythmia / flutter, are:
- Pulse measurement.
- Electrocardiogram (ECG).
- Dynamic electrocardiogram according to Holter.
- Chest X-ray.
- Echocardiography
Pulse measurement. The cardiologist can draw fundamental information from the evaluation of:
- Arterial pulse. The measurement is made on the radial artery. It informs about the frequency and regularity of the heart rhythm.
- Jugular venous pulse. It is useful for understanding the level of venous pressure.
Electrocardiogram (ECG). It is the instrumental examination indicated to evaluate the course of the electrical activity of the heart. Based on the traces that result, the doctor can recognize and distinguish an atrial flutter from atrial fibrillation.
Dynamic electrocardiogram according to Holter. It is a normal ECG, with the advantageous difference that the monitoring lasts for 24-48 hours, without preventing the patient from carrying out normal activities of daily life. It is useful when episodes of atrial flutter are sporadic and unpredictable.
Chest X-ray. It is a "clinical investigation that aims to understand if there are particular pulmonary and respiratory diseases.
Echocardiography. Using the ultrasound emission, this non-invasive investigation shows the fundamental elements of the heart: atria, ventricles and valves. The evaluation of the heart allows to verify the presence of a valvulopathy or some other cardiac malformation.
Therapy
Therapy depends on the form of atrial flutter and the state of health of the person affected by the arrhythmic episodes.
If it is a paroxysmal flutter, it is done in the following way:
- Administration of drugs:
- Digital. Slow down your heart rate
- Antiarrhythmics: quinidine derivatives, dofetilide, ibutilide, flecainide, propafenone and amiodarone. They serve to normalize the heart rhythm.
- Electrical treatment:
- Cardioversion. Non-invasive technique, which infuses an electrical discharge, called shock, in order to reset the altered heart rhythm and restore the normal beat, marked by the sinoatrial node.
Maintenance treatments, always based on digitalis and antiarrhythmics, are also indicated to prevent other paroxysmal episodes, especially if it is certain that the patient suffers from hyperthyroidism or hypertension.
However, it is important to point out that some circumstances, such as:
- Tolerable symptoms.
- Spontaneous resolution, in the past, of other episodes of atrial flutter.
- Absence of cardiac and non-cardiac pathologies.
make therapy unnecessary. This is to avoid any side effects related to drug intake, such as quinidine gastrointestinal disorders.
If the atrial flutter is permanent, it very often means that the "origin of the disorder" is a heart disease or other pathology. Resolving this condition, with a therapeutic approach chosen on a case-by-case basis, is the fundamental step to help restore normal heart rhythm. The therapy, on the other hand, aimed at treating atrial flutter, acts as a support and maintenance. It is as follows:
- Administration of drugs:
- Digital.
- Antiarrhythmics: quinidine derivatives, dofetilide, ibutilide, flecainide, propafenone and amiodarone.
- Anticoagulants. The permanent forms can create a situation of thrombo-embolism. They are used in the presence of particular heart disease, mitral valve disease, which could generate thrombi or emboli.
- Beta-blockers and calcium channel blockers. They slow down the heart rhythm, acting at the level of the atrioventricular node. They are administered to those who are tolerant to digitalis.
- Electrical treatment:
- Cardioversion. It is no longer indicated when the patient has a heart disease that alters the structure of the heart, such as valvulopathies.
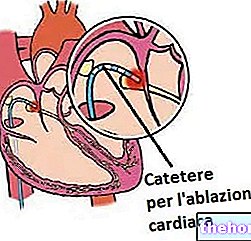
- Catheter radiofrequency ablation. A catheter is used which, once conducted to the heart, is able to infuse a radiofrequency discharge by hitting the area of myocardium that generates the atrial flutter. The affected area is destroyed and this should rearrange the number of impulses contraction by the sinoatrial node is an invasive technique.
See Also: Drugs to Treat Atrial Flutter "