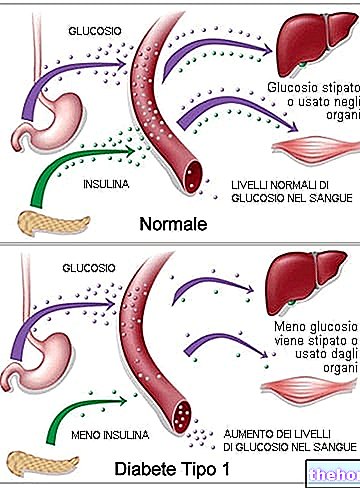
Let us briefly recall that insulin is an essential hormone to allow the passage of glucose from the blood to the cells, preventing its blood concentration (glycaemia) from rising too high. Not all body cells need insulin to absorb glucose; "hormone, however, is essential for muscle and adipose tissue, which alone account for about 60% of body mass.
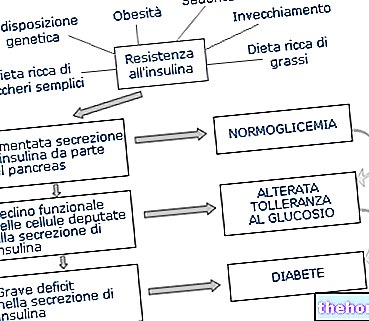
In response to insulin resistance, the body puts in place a compensatory mechanism based on the increased release of insulin; in these cases, we speak of hyperinsulinemia, ie high levels of the hormone in the blood. If in the initial stages this compensation is able to maintain blood sugar at normal levels (euglycemia), in an advanced stage the pancreatic cells responsible for producing insulin are unable to adapt its synthesis; the result is an increase in post-prandial blood glucose.

Finally, in the full-blown phase, the further reduction in plasma insulin concentration - due to the progressive exhaustion of pancreatic beta-cells - determines the onset of hyperglycemia even in fasting conditions.
Not surprisingly, therefore, insulin resistance is often the antechamber of diabetes.
To understand the biological reasons behind this negative evolution it is necessary to have sufficient knowledge on the regulatory mechanisms of glycemia and on the hormones that participate in it. Briefly, insulin resistance determines:
- an increase in the hydrolysis of triglycerides in the adipose tissue, with an increase in fatty acids in the plasma;
- a decrease in glucose uptake in the muscles, with a consequent decrease in glycogen deposits;
- a greater hepatic synthesis of glucose in response to the "increased concentration of fatty acids in the blood and the disappearance of the processes that inhibit it; consequently there is an increase in fasting glycemic levels.
- it is believed that compensatory hyperinsulinemia renders the beta-cell unable to activate all those molecular mechanisms necessary for its proper functioning and its normal survival. The decreased functionality of the pancreatic cells responsible for insulin synthesis opens the doors to type II diabetes mellitus .
Muscle tissue is the main site of peripheral insulin resistance; however, during physical activity this tissue loses its dependence on insulin and glucose is able to enter muscle cells even in the presence of particularly low insulin levels.
, cortisol and glucagon, capable of antagonizing the action of insulin, to the point of determining insulin resistance when present in excess (as typically occurs in Cushing's syndrome).
The ways in which these hormones oppose insulin are the most disparate: for example, they can act on insulin receptors by reducing their number (this is the case of GH), or on the transduction of the signal grafted by the insulin-receptor bond (necessary to regulate the cellular response). This last biological action consists in the redistribution of glucose transporters GLUT4 * from the intracellular compartment to the plasma membrane; all this allows to increase the supply of glucose. Even the exogenous supply of these hormones (for example cortisone or growth hormone) can determine insulin resistance. There may also be genetic causes caused by mutations in the insulin receptor. In most cases, however, the causes of insulin resistance are not clearly determinable.
In addition to the inevitable hereditary component, in most cases insulin resistance affects people affected by diseases and conditions such as hypertension, obesity (especially android or abdominal), pregnancy, fatty liver, metabolic syndrome, use of anabolic steroids, atherosclerosis, polycystic ovary syndrome, hyperandrogenism and dyslipidemia (high values of tiglycerides and LDL cholesterol associated with a reduced amount of HDL cholesterol). These conditions, associated with the inevitable genetic component, also represent possible causes / consequences of insulin resistance and are important for its diagnosis.
.
Sometimes the classic glycemic curve is also used, which in the presence of insulin resistance presents a relatively normal trend, only to present - after several hours - a rapid decline in glycaemia (due to hyperinsulinemia).
. Also useful are the aids capable of reducing or slowing down the intestinal absorption of sugars (acarbose and fiber supplements such as glucomannan and psyllium). Some drugs used in the treatment of diabetes, such as metformin, have also proved effective in the treatment of "insulin resistance; however, it is very important to intervene first of all on the diet and the level of physical activity, resorting to drug therapy only when lifestyle changes are not sufficient.* Muscle and fat tissue cells "absorb" blood glucose through the plasma membrane. It is a process of facilitated diffusion carried out by a family of glucose transporters, partly present constitutively on the cell surface (GLUT1) and partly translocated on the membrane in response to different stimuli (GLUT4). Among these stimuli, the most powerful and known is represented by insulin.