Generality
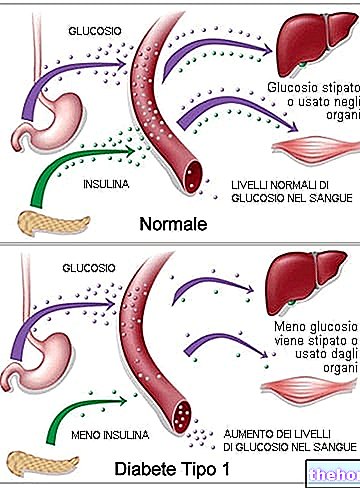
Type 1 diabetes mellitus is a metabolic disorder caused by a lack (or severe insufficiency) of insulin, a hormone produced by the pancreas.
The classic symptoms mainly concern increased urination, thirst and appetite, and weight loss.

The underlying causes of this autoimmune reaction are poorly understood; it is assumed that they may be of a genetic type or of endogenous or exogenous stress.
The main test that allows to diagnose type 1 diabetes mellitus, and to distinguish it from type 2 diabetes, is based on the search for the autoantibodies involved in the autoimmune reaction.
To live, the type 1 diabetic requires the administration of exogenous insulin, that is a synthetic form of the hormone, similar to the natural one. This therapy must be followed indefinitely and, in general, does not compromise normal daily activities. All type 1 diabetics are educated and trained in self-management of insulin drug therapy.
Left untreated, type 1 diabetes mellitus causes various serious complications, both acute and chronic. Other complications of type 1 diabetes mellitus are collateral in nature and are mainly based on hypoglycaemia caused by the administration of an excessive dose of insulin.
Type 1 diabetes mellitus accounts for 5-10% of overall diabetes cases worldwide.
Pancreas and Type 1 Diabetes Mellitus
Brief Anatomo-Functional Recall
The pancreas is a glandular organ that intervenes by supporting the digestive system and the endocrine system of vertebrates.
In humans, it is found in the abdominal cavity, behind the stomach.
It is an endocrine gland that produces several important hormones, including insulin, glucagon, somatostatin and pancreatic polypeptide.
It also plays an exocrine role, as it secretes a digestive juice containing specific enzymes for the digestion of carbohydrates, proteins and lipids in the chyme.
In type 1 diabetes mellitus only the endocrine function of insulin is compromised.
Pathophysiology
Type 1 (also known as T1D) is a form of diabetes mellitus caused by the autoimmune lesion of the beta cells of the pancreas. Once damaged, these cells no longer produce insulin, no matter what the risk factors and the causative entities may be.
In the past, type 1 diabetes mellitus was also referred to as insulin-dependent or juvenile diabetes, but today these definitions are considered fundamentally incorrect or incomplete.
The individual causes of type 1 diabetes mellitus can relate to various pathophysiological processes which, in turn, destroy the beta cells of the pancreas. The process takes place through these steps:
- Recruitment of autoreactive CD4 helper T cells and cytotoxic CD8 T cells
- Recruitment of autoantibodies B
- Activation of the innate immune system.

Causes
The causes of type 1 diabetes mellitus are unknown.
Several explanatory theories have been advanced and the causes may be one or more of those we are going to list:
- Genetic predisposition
- Presence of a diabetogenic activator (immune factor)
- Exposure to an antigen (e.g. a virus).
Genetics and Inheritance
Type 1 diabetes mellitus is a disease involving more than 50 genes.
Depending on the locus or the combination of loci, the disease can be: dominant, recessive or intermediate.
The strongest gene is IDDM1 and is found on chromosome 6, more precisely in the 6p21 staining region (MHC class II). Some variants of this gene increase the risk of decreased type 1 histocompatibility characteristic. These include: DRB1 0401, DRB1 0402, DRB1 0405, DQA 0301, DQB1 0302 and DQB1 0201, which are more common in European and North American populations. Remarkably, some appear to play a protective role.
A child's risk of developing type 1 diabetes mellitus is:
- 10% if the father is affected
- 10% if the brother is affected
- 4% if the mother is affected and was 25 or younger at the time of delivery
- 1% if the mother is affected and was over 25 at the time of delivery.
Environmental factors
Environmental factors influence the expression of type 1 diabetes mellitus.
For monozygotic twins (who have the same genetic heritage), when one of the two is affected by the disease, the other has only a 30-50% chance of manifesting it. This means that in 50-70% of cases the disease attacks only one of the two identical twins. The so-called concordance index is less than 50%, suggesting a VERY important "environmental influence.
Other environmental factors refer to the residential area. Certain European areas, in which Caucasian populations reside, have a 10 times higher risk of onset than many others. In the event of a relocation, the danger appears to increase or decrease based on the country of destination.
Role of Viruses
A theory on the causes of the onset of type 1 diabetes mellitus is based on the interference of a virus. This would trigger the immune system which, for still mysterious reasons, ends up attacking also the beta cells of the pancreas.
The viral family Coxsackie, to which the rubella virus belongs, appears to be involved in this mechanism but the evidence is not yet sufficient to prove it. In fact, this susceptibility does not affect the whole population and only some subjects affected by rubella develop type 1 diabetes mellitus.
This suggested a certain genetic vulnerability and, not surprisingly, the hereditary tendency of particular HLA genotypes was identified. However, their correlation and autoimmune mechanism remain misunderstood.
Chemicals and Drugs
Some chemicals and certain drugs selectively destroy pancreatic cells.
The pyrinurone, a rodenticide released in 1976, selectively destroys pancreatic beta cells causing type 1 diabetes mellitus. This product was withdrawn from most markets in the late 1970s, but not everywhere.
There streptozotocin, an antibiotic and anticancer agent used in chemotherapy for pancreatic cancer, kills the organ's beta cells by depriving it of the endocrine capacity for insulin.
Symptoms
Classic symptoms of type 1 diabetes mellitus include:
- Polyuria: excessive urination
- Polydipsia: increased thirst
- Xerostomia: dry mouth
- Polyphagia: increased appetite
- Chronic fatigue
- Unjustified weight loss.

Acute Complications
Many type 1 diabetics are diagnosed at the onset of certain complications typical of the disease, such as:
- Diabetic ketoacidosis
- Non-ketotic hyperosmolar-hyperglycemic coma.
Diabetic Ketoacidosis: How Does It Occur?
The ketoacidosis of type 1 diabetes mellitus occurs due to the accumulation of ketone bodies.
These are metabolic wastes induced by the consumption of fats and amino acids for energy purposes. This circumstance is manifested by the lack of insulin and the consequent deficit of glucose in the tissues.
The signs and symptoms of diabetic ketoacidosis include:
- Xeroderma: dry skin
- Hyperventilation and tachypnea: deep and rapid breathing
- Drowsiness
- Abdominal pain
- He retched.
Non-ketotic Hyperosmolar-Hyperglycemic Coma
Very often triggered by an "infection or by taking drugs in the presence of type 1 diabetes mellitus, it has a mortality of up to 50%.
The pathological mechanism provides:
- Excessive glycemic concentration
- Intense renal filtration for glucose excretion
- Lack of rehydration.
It often presents with the appearance of focal or generalized seizures.
Chronic Complications
The long-term complications of type 1 diabetes mellitus are mainly related to macro and micro angiopathies (complications of the blood vessels).
Complications of poorly managed type 1 diabetes mellitus can include:
- Vascular diseases of the macrocirculation (macroangiopathies): stroke, myocardial infarction
- Vascular diseases of the microcirculation (microangiopathies): retinopathies, nephropathies and neuropathies
- Others, related or unrelated to the above: diabetic kidney failure, sensitivity to infections, diabetic foot amputation, cataracts, urinary tract infections, sexual dysfunction etc.
- Clinical depression: in 12% of cases.
The pathological basis of macroangiopathies is that of atherosclerosis.
However, cardiovascular disease and neuropathy can also have an autoimmune basis. For this type of complication, women have a 40% higher risk of death than men.
Infections of the Urinary Tract
People with type 1 diabetes mellitus show an increased rate of urinary tract infections.
The reason is bladder dysfunction related to diabetic nephropathy. This can cause a decrease in sensitivity which, in turn, leads to an increase in urinary retention (risk factor for infections).
Sexual Dysfunction
Sexual dysfunction is often the result of physical factors (such as nerve damage and / or poor circulation) and psychological factors (such as stress and / or depression caused by the demands of the disease).
- Males: the most common sexual problems in males are erection and ejaculation difficulties (retrograde complication).
- Female: Statistical studies have shown the existence of a significant correlation between type 1 diabetes mellitus and sexual problems in women (although the mechanism is unclear). The most common dysfunctions include reduced sensitivity, dryness, difficulty / inability achieving orgasm, pain during sex and decreased libido.
Diagnosis
Type 1 diabetes mellitus is characterized by recurrent and persistent hyperglycemia, which can be diagnosed with one or more of the following requirements:
- Fasting blood glucose equal to or greater than 126mg / dL (7.0mmol / L)
- Blood glucose equal to or greater than 200mg / dl (11.1mmol / L), 2 hours after oral administration of an oral load equal to 75g of glucose (glucose tolerance test)
- Hyperglycemia Symptoms and Diagnostic Confirmation (200mg / dL or 11.1mmol / L)
- Glycated hemoglobin (type A1c) equal to or greater than 48mmol / mol.
NB. These criteria are recommended by the World Health Organization (WHO).
Debut
About ¼ of patients with type 1 diabetes mellitus begin with diabetic ketoacidosis. This is defined as a "metabolic acidosis caused by" the increase of ketone bodies in the blood; this increase is in turn caused by the exclusive energy use of fatty acids and amino acids.
More rarely, type 1 diabetes mellitus may begin with hypoglycemic collapse (or coma). This is due to the excessive production of insulin in the few moments before the final interruption. This is a rather dangerous circumstance.
Differential diagnosis
Diagnosis of other types of diabetes occurs under different circumstances.
For example, with ordinary screeneng, with the random detection of hyperglycemia and through the recognition of secondary symptoms (fatigue and visual disturbances).
Type 2 diabetes is often identified belatedly for the onset of long-term complications, such as: stroke, myocardial infarction, neuroparies, foot ulcers or difficulty in healing wounds, eye problems, fungal infections and childbirth suffering from macrosomia or hypoglycemia.
A positive result, in the absence of unequivocal hyperglycemia, must in any case be confirmed by the repetition of a positive result.
The differential diagnosis between type 1 and type 2 diabetes mellitus, both characterized by hyperglycemia, mainly concerns the cause of the metabolic impairment.
While in type 1 there is a significant reduction in insulin due to the destruction of pancreatic beta cells, in type 2 there is insulin resistance (absent in type 1).
Another factor that characterizes type 1 diabetes mellitus is the presence of antibodies aimed at the destruction of pancreatic beta cells.
Autoantibody Detection
The appearance in the blood of autoantibodies linked to type 1 diabetes mellitus has been shown to be able to predict the onset of the disease even before hyperglycemia.
The main autoantibodies are:
- Islet cell autoantibodies
- Insulin autoantibodies
- Autoantibodies targeting the 65 kDa isoform of glutamic acid decarboxylase (GAD),
- Tyrosine-phosphatase anti-IA-2 autoantibodies
- Zinc transporter 8 autoantibodies (ZnT8).
By definition, the diagnosis of type 1 diabetes CANNOT be made before the onset of symptoms and clinical signs. However, the appearance of autoantibodies can still delineate a condition of "latent autoimmune diabetes".
Not all subjects who show one or some of these autoantibodies develop type 1 diabetes mellitus. The risk increases as they increase; for example, with three or four different types of antibodies a risk level of 60- is reached. 100%.
The time interval between the appearance of autoantibodies in the blood and the onset of clinically diagnosable type 1 diabetes mellitus can be a couple of months (infants and young children); on the other hand, in some individuals it can take several years.
Only the assay of anti-islet cell autoantibodies requires conventional immunofluorescence detection, while the others are measured with specific radiobinding tests.
Prevention and Therapy
Type 1 diabetes mellitus is currently not preventable.
Some researchers argue that it could be avoided if properly treated in its latent autoimmune phase, before the immune system activates against pancreatic beta cells.
Immunosuppressive drugs
It seems that the cyclosporine A, an immunosuppressive agent, is capable of blocking the destruction of beta cells. However, its renal toxicity and other side effects make it highly inappropriate for long-term use.
Anti-CD3 antibodies, including the teplizumab and the "otelixizumab, appear to preserve insulin production. The mechanism of this effect is probably attributable to the conservation of regulatory T cells. These mediators suppress the activation of the immune system, maintain homeostasis and tolerance of self-antigens. The duration of these effects is still unknown
The anti-CD20 antibodies of the rituximab they inhibit B cells, but the long-term effects are unknown.
Diet
Some research has suggested that breastfeeding reduces the risk of developing type 1 diabetes mellitus.
Intake of vitamin D of 2000 IU in the first year of life has been shown to be preventive, but the causal relationship between the nutrient and disease is unclear.
Children with antibodies against beta cell proteins, when treated with vitamin B3 (PP or niacin), show a drastic reduction in incidence over the first seven years of life.
Stress and Depression
The psychological stress linked to the lifestyle of the type 1 diabetic is of considerable magnitude; not surprisingly, the complications of this pathology also include depressive symptoms and major depression.
To avoid this, there are preventive measures including: exercise, hobbies and participation in charities.
Insulin
In contrast to type 2 diabetes mellitus, diet and exercise are not a cure.
For endocrine insufficiency, type 1 diabetics are forced to inject insulin subcutaneously or through pumping.
Today, insulin is synthetic in nature; in the past, hormones of animal origin (cattle, horses, fish, etc.) have been used.
There are four main types of insulin:
- Fast-acting: the "effect sets in in 15" minutes, peaking between 30 and 90 ".
- Short-acting: the "effect sets in in 30" minutes, peaking between 2 and 4 hours.
- Intermediate action: the effect occurs in 1-2 hours, with a peak between 4 and 10 hours.
- Long-acting: administered once a day, it has an effect that occurs in 1-2 hours, with a "prolonged action that lasts for all 24.
ATTENTION! An excess of insulin can induce hypoglycemia (
Dietary management and blood glucose detection are two very important factors that serve to avoid excess and defect of exogenous insulin.
Regarding the diet, one of the cornerstones is the carbohydrate counting; for what concerns the glycemic estimate, however, it is sufficient to use an electronic device (glucometer).
See also: Type 1 diabetes mellitus diet.
The goal of dietary / hormonal management is to keep glycaemia around 80-140mg / dl in the short term and glycated hemoglobin below 7%, in order to avoid long-term complications.
For further information: Drugs for the Treatment of Type 1 Diabetes "
Pancreas transplant
In type 1 diabetes mellitus, especially in cases where insulin therapy is more difficult, it is also possible to perform a transplant of beta cells in the pancreas.
The difficulties are related to the recruitment of compatible donors and the side effects in the use of anti-rejection drugs.
The success rate in the first 3 years (defined as insulin independence) is estimated to be around 44%.
Epidemiology
Type 1 diabetes accounts for 5-10% of all diabetes cases, or 11-22 million worldwide.
In 2006, type 1 diabetes mellitus affected 440,000 children under the age of 14 and was the primary cause of diabetes in those under the age of 10.
Diagnosis of type 1 diabetes mellitus increases by about 3% every year.
Rates vary greatly from country to country:
- In Finland, 57 cases per 100,000 per year
- In Northern Europe and the United States, 8-17 cases per 100,000 per year
- In Japan and China, 1-3 cases per 100,000 per year.
Asian Americans, Hispanic Americans, and Hispanic Americans of color are more likely to get type 1 diabetes mellitus than non-Hispanic whites.
Research
Type 1 diabetes research is funded by governments, industry (eg, pharmaceutical companies) and charities.
Currently, the experimentation is moving in two different directions:
- Pluripotent stem cells: These are cells that can be used to generate additional specific beta cells. In 2014, an experiment on mice gave a positive result but, before these techniques can be used in humans, more research is needed.
- Vaccine: Vaccines to treat or prevent type 1 diabetes are designed to induce immune tolerance on pancreatic beta cells and insulin. After some unsuccessful outcomes, there is currently no working vaccine. New protocols have been initiated since 2014.




.jpg)