Generality
Diabetic ketoacidosis is a serious complication of diabetes mellitus, in particular of insulin-dependent diabetes (type I and more rarely type II); it is in fact caused by an absolute deficiency of insulin, in response to which the organism produces significant quantities of ketone bodies.

Causes
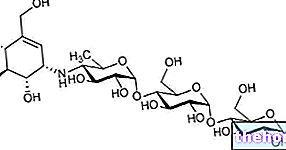
When glucose fails to enter the cells, they adapt to use mainly fatty acids, whose metabolism - in the absence of adequate intracellular amounts of glucose - turns towards the synthesis of substances called ketones or ketone bodies.
At the same time, given the lack of sugar, we are absurdly witnessing an "exalted secretion of counterinsular hormones (glucagon, catecholamines, cortisol and GH), which stimulate the synthesis of glucose (gluconeogenesis and glycogenolysis); the newly formed sugar is then poured into the circulation where, not being able to enter the cells due to the absence of insulin, it aggravates the hyperglycemic condition.
The accumulation of ketone bodies in the blood, hyperglycemia and insulin deficiency, therefore determine the characteristic symptoms and complications of diabetic ketoacidosis, which in extreme situations can be even fatal.
Diabetic ketoacidosis is an acute complication of diabetes mellitus, which causes hyperglycemia (high blood glucose levels), ketonemia (accumulation of ketone bodies in the blood) and metabolic acidosis.
Differences from ketosis in healthy people
A similar situation, but much less serious (we are simply talking about ketosis and not ketoacidosis), occurs in people who follow a particularly low-carbohydrate diet or have been fasting for a long time.
The difference between these situations and the ketoacidosis of diabetics is that the latter, not producing insulin, are unable to regulate the synthesis of ketone bodies, which becomes exasperated and out of control; moreover, due to the inability to let glucose enter the cells, they find themselves in the paradox of synthesizing ketone bodies in conditions of hyperglycemia, which, as in the most vicious of circles, is further increased by the secretion of counterinsular hormones.
Symptoms
For further information: Diabetic Ketoacidosis Symptoms
In diabetic ketoacidosis it is therefore the coupled hyperglycemia / ketosis that reduces the blood pH and causes symptoms such as vomiting, dehydration, polyuria (frequent and copious urination), polydipsia (intense thirst), hypotension, arrhythmias, deep and panting breathing, drowsiness and state confusional up to coma. The breath of a person affected by diabetic ketoacidosis also assumes the typical smell of ripe fruit; it is a symptom linked to the elimination of acetone, a ketone body deriving from the degradation of acetoacetic acid (one of the three ketone bodies together with B-hydroxybutyrate and the aforementioned acetone).
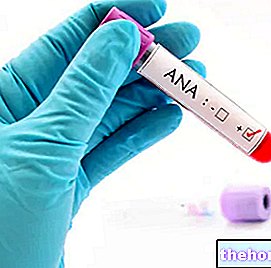
Diagnosis
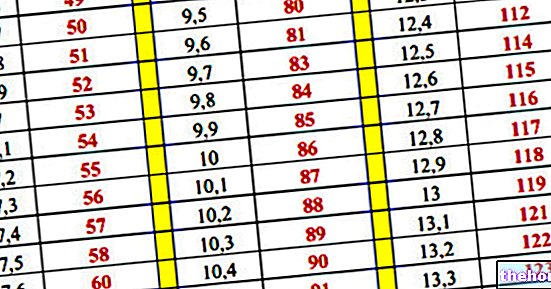
Clinically, in the patient with diabetic ketoacidosis there is hyperglycemia, hypovolemia, reduction of blood bicarbonate, presence of ketone bodies in the blood (ketonemia) and urine (ketonuria), electrolyte alterations and reduction of blood pH.
Ketoacidosis can be found at onset, that is, when type 1 diabetes occurs for the first time (usually at a young age), or following a deliberate abstention from insulin therapy.
Precipitating factors, which can favor its onset, are represented by concomitant infections, malfunctioning of the insulin pump and more generally by important physical and psychological stress (trauma, myocardial infarction, acute cerebro-vascular episode, etc.). ).
Treatment
The treatment of diabetic ketoacidosis, to be performed in a hospital setting, involves the intravenous administration of fluids to resolve dehydration, and insulin to stop the synthesis of ketone bodies. Also important is the monitoring and possible correction of electrolyte imbalances.
Specific treatments can also be undertaken against underlying infections (such as pneumonia or urinary infections), which often constitute an aggravating situation; stress, in fact, increases the secretion of hyperglycemic hormones such as cortisol and catecholamines.
In these situations, the patient may also be led to think that - due to poor appetite and poor food intake - it is necessary to reduce the insulin dose; in the face of such occurrences, to prevent diabetic ketoacidosis, it is instead important to intensify glycemic controls and adapt the therapeutic scheme as recommended by the diabetologist.