Generality
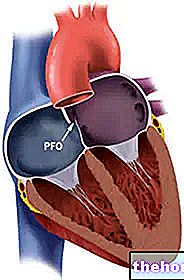
Pericarditis is inflammation of the pericardium, that is the membrane that surrounds, supports and protects the heart. The causes of this disorder are various, sometimes not recognizable even after an accurate diagnosis.

The therapy consists of different pharmacological treatments, applied according to the characteristics of the pericarditis. Surgery is required only in extreme conditions.
What is the pericardium?
The pericardium is the membrane that surrounds the heart and the root of the main blood vessels that branch off from it (aorta, pulmonary arteries, hollow veins and pulmonary veins). The pericardium is made up of two layers, separated from each other by the pericardial fluid.
The outermost layer is the so-called fibrous pericardium.
The innermost layer, on the other hand, is the serous pericardium; it adheres perfectly to the heart and all its inlets and is made up of two sheets of cellular tissue, called the parietal sheet and the visceral sheet.

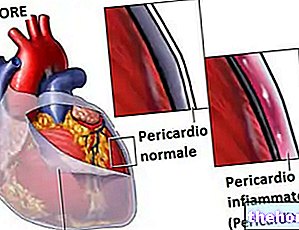
Figure: the pericardium: location and anatomy. From the site: anunexpectederror.blogspot.it
The pericardial fluid, whose normal volume is about 20-50ml, serves to reduce the friction and friction of the two layers making up the pericardium.
FUNCTIONS OF THE PERICARDIUM
In addition to acting as a lubricant, the pericardium has several other functions.
It is essential to fix and maintain the heart in the correct position inside the mediastinum. It acts as a defensive barrier against infections, viral or bacterial, which could compromise cardiac activity. Finally, it avoids the excessive dilation of the heart, when it is affected by particular pathologies.
What is pericarditis?
With the term pericarditis it refers to the inflammation of the pericardium, that is the thin membrane that wraps and protects the heart.
Inflammation of the pericardium is characterized by irritation, swelling and sometimes effusion: in other words, the so-called inflammatory edema.
Pericarditis manifests itself with chest pain, very similar (in some respects) to that caused by a heart attack or lung disease. However, unlike these pathological situations, it is less severe.
TYPES OF PERICARDITIS
There are several types of pericarditis:
- Acute pericarditis
Acute is defined when symptoms last less than three months. Acute-type disorder typically resolves within a few weeks with proper treatment. - Recurrent pericarditis
It is defined as recurrent, when the patient is suffering from several consecutive acute pericarditis. - Chronic pericarditis
Chronic is defined when symptoms last more than three months. It is considered a complication of acute pericarditis.
EPIDEMIOLOGY

Figure: Comparison between a normal heart (left) and heart with pericardial effusion (right). The arrows indicate the pressure that the accumulated fluid exerts on the heart. From the site: cardiachealth.org
Pericarditis is a common condition, but it is not always diagnosed. The lack of recognition is due to different reasons: it can be a consequence of a more serious pathology or it can resolve spontaneously in a few days, without alarming the patient.
Pericarditis is a disorder that can arise at any age; however, the most affected individuals are adults, between the ages of 20 and 50.
Men are generally more affected than women. Furthermore, people affected by a first episode of pericarditis are more likely to experience similar events in the future (recurrent pericarditis).
Causes
Pericarditis pain arises as a result of a change in the composition of the pericardial fluid. The latter, in fact, by filling with inflammatory cells, compromises its lubricating function and causes friction and friction to be created between the fibrous and serous layers; friction and friction, which manifest themselves precisely with the painful sensation.
In addition, it can sometimes happen that the liquid increases in volume, thus exerting painful pressure on the heart. This situation is also known by the term pericardial effusion.
POSSIBLE CAUSES
The possible causes of pericarditis and their mechanisms of action are now almost completely known. What is still problematic, in some cases, is the exact recognition of the specific cause. This uncertainty remains even after having subjected a patient to a detailed diagnosis.
It is for this reason, therefore, that very often we speak of idiopathic pericarditis, referring, with this term, to the fact that we are not able to establish the precise reason, among the many hypothesized.
Usually, the "origin of the disorder c" is a "viral infection, but bacterial infections, autoimmune diseases, tumors, renal failure, etc. cannot be ruled out.
WHEN THE CAUSE IS A VIRAL INFECTION
The most common viral infections are those sustained by enteroviruses. Often, these viruses manifest themselves, first, with a cold or with meningitis and, later, with a pericarditis.
Alongside enteroviruses, there are: adenoviruses, that is, those that also cause pneumonia, bronchitis and some forms of myocarditis; the Epstein-Barr virus; cytomegaloviruses; some herpes simplex viruses; influenza viruses; the hepatitis C virus; the AIDS virus.
THE LESS COMMON CAUSES
Pericarditis, as anticipated, in addition to viruses, can also be caused by other causes. These are less common, but equally important situations.
- Bacterial infections
It has been found that individuals with tuberculosis often develop pericarditis at the same time or later. - Autoimmune Diseases
An autoimmune disease arises when an organism's immune system turns against the organism, attacking its organs. An association has been observed between pericarditis and rheumatoid arthritis, lupus and scleroderma. - Radiotherapy
People affected by lung cancer and undergoing radiotherapy are more exposed to pericarditis. - Kidney failure
An "association between the two disorders has been established, but the reason is unclear. - Hypothyroidism
As with kidney failure, a link has been found between the two conditions, but the reason is not known. - Tumors
Several cancers, especially when they spread with metastases to the rest of the body, also result in pericarditis. - Heart attack
A heart attack can cause inflammation of the pericardium at the time of its onset or even months later. If it occurs later, it is referred to as Dressler's syndrome. - Pulmonary embolism
The presence of a pulmonary embolus can also manifest itself with pericarditis. - Complications of heart surgery
A "heart surgery can cause, as a complication, an" inflammation of the layers of the pericardium. - Complications of a car accident
The cause of pericarditis is, in these cases, thoracic trauma. - Complications from taking medications
Certain drugs, such as penicillin, phenytoin (anticonvulsant), warfarin (anticoagulant), procainamide (antiarrhythmic) and some anti-cancer drugs, have been observed to cause inflammation of the pericardium in some individuals.
CAUSES OF RECURRING PERICARDITIS
Recurrent type pericarditis is a curious case, as the mechanism that causes them is not yet clear.
A first theory holds that at the origin there is an abnormal and delayed immune response. In some respects, this hypothesis is reminiscent of an autoimmune disease, in which antibodies attack the organism that they are supposed to defend. In recurrent pericarditis, this phenomenon appears to occur from time to time.
A second theory maintains that the abilities possessed by some viruses allow them to "hide" in the cells of the pericardium and reveal themselves after months, in a repeated way.
Finally, the third theory sees corticosteroid drugs at the center of attention. According to a statistic, in fact, it emerged that patients with pericarditis, treated with these drugs, are more exposed to subsequent relapses.
Symptoms and Complications
For further information: Pericarditis Symptoms
The main symptom, whatever the cause that triggered the pericarditis, is chest pain, felt just behind the breastbone.
The rest of the symptoms depend on the reasons that caused the inflammation of the pericardium: the patient, depending on the case, can therefore manifest fever, fatigue, shortness of breath, etc.
THE CHEST PAIN
Chest pain from pericarditis is sudden, sharp, and excruciating. Usually, it is felt behind the breastbone, on the left side. In some cases, it can branch out to the right shoulder and neck.
Some patients describe the pain as a discomfort that produces a sense of pressure in the chest.
Coughing, breathing deeply, eating or lying down are acts that exacerbate the painful sensation. Conversely, sitting or bending forward are postures that produce relief.
Chest pain from pericarditis and heart attack pain are very similar, so much so that it is impossible to recognize them, except with appropriate diagnostic investigations. Therefore, although pericarditis is not a particularly serious pathological condition (except for those forms sustained by serious pathological conditions, such as a tumor, a heart problem, etc.), chest pain like the one just described deserves great attention, both from who is affected is by the doctor.
OTHER SYMPTOMS
Depending on the causes that caused pericarditis, the patient may experience the following symptoms and signs:
- High fever
- Shortness of breath
- Fatigue and a sense of weakness
- Nausea
- Dry cough
- Swelling in the legs or abdomen
SYMPTOMS OF RECURRING PERICARDITIS
Recurrent pericarditis can present itself in two ways: persistent or intermittent.
It is persistent, when symptoms appear shortly after stopping drug treatments (for example, NSAIDs).
It is of the intermittent type, however, when the symptoms reappear after months, if not years. Often, in these cases, we come across the so-called Dressler syndrome, the root cause of which is a heart attack.
COMPLICATIONS
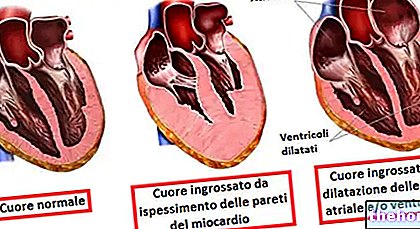
Chronic pericarditis is considered a complication of acute-type pericarditis. It is defined as chronic when the symptoms and signs it causes last for more than three months.
There are two forms of chronic pericarditis:
- Chronic exudative pericarditis
Features: inside the pericardium there is a small excess of fluid (pericardial effusion), due to inflammation. The quantities are modest, but they cause persistent pain, fainting and shortness of breath.
Causes: tuberculosis, hepatitis, tumor metastases and complications after heart surgery. Sometimes, there is no clear explanation. - Chronic constrictive pericarditis
Features: Prolonged inflammation can stiffen the membrane that makes up the pericardium and cause it to lose elasticity. In doing so, the heart struggles to perform its pumping action because it can no longer fill with blood and contract as it should. The classic symptoms are shortness of breath, fatigue, abdominal pain, nausea and vomiting.
Causes: tuberculosis, effects of radiotherapy and complications after heart surgery. Sometimes, there is no clear explanation.
Alongside these two particularly serious forms of chronic pericarditis, which can endanger the patient's life (or at least require surgery), there is a third equally serious complication: the so-called cardiac tamponade.
Symptoms and signs of cardiac tamponade:
- Hypotension (drop in blood pressure, due to reduced blood supply)
- Feeling of fainting
- Blurred vision
- Palpitations
- Confusion
- Nausea
- General weakness
- Loss of consciousness
The condition of cardiac tamponade occurs when the pericardial fluid increases in a very high way (severe pericardial effusion), so much so that the activity of the heart is seriously compromised. In some respects, it resembles chronic exudative pericarditis, but with even more dramatic effects: the patient, in fact, suffers from numerous ailments and needs an appropriate surgical intervention.The most common causes are tuberculous bacterial infections and tumor metastases.
WHEN TO SEEK YOUR DOCTOR
It is advisable to consult a doctor when chest pain occurs in the ways described above: sudden, sharp, stabbing and as a sense of pressure. In fact, although pericarditis is not in itself a serious pathological condition, it still deserves due attention, because it could originate from much more dangerous circumstances (heart attack, pulmonary embolism, etc.).
Diagnosis
The first step in establishing a correct diagnosis of pericarditis is a complete physical examination of the patient. After that, more specific checks are carried out, such as blood tests and instrumental tests.
OBJECTIVE EXAMINATION
The physical examination begins with the anamnesis, that is, with the collection of information relating to symptoms and clinical history directly from the voice of the patient (or family members).
The doctor then asks the patient several questions to understand whether one of the above causes of pericarditis has occurred in the recent past (viral infection, bacterial infection, car accident, heart surgery, etc.).
After that, we proceed with the stethoscopic check. Cardiac auscultation, using a stethoscope, allows you to recognize a harsh noise, like something scratching. This noise is the result of the rubbing between the two layers of pericardium and the abnormal pericardial fluid.
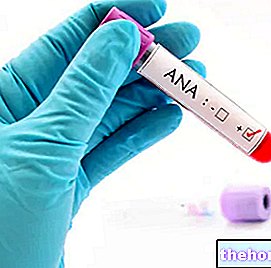
BLOOD TESTS
The checks on a blood sample are used to trace the possible presence of infections (viral or bacterial) in progress. In addition, it can also be useful to take and analyze a sample of pericardial fluid, since it can provide a lot of information.
INSTRUMENTAL EXAMINATIONS

Figure: Chest x-ray of a person with pericarditis. From the site: circ.ahajournals.org
Instrumental tests are essential to confirm the pre-diagnosis and not only: through them, in fact, the anomalies at the level of the pericardium, the triggering causes and the possible related pathologies are clarified.
- Electrocardiogram (ECG). By applying electrodes to an individual's skin, the electrical activity of the heart is measured. If the person being tested actually has pericarditis, the doctor recognizes specific abnormalities in the heartbeat.
- Chest X-ray. It allows you to evaluate the shape and size of the heart. The heart of a patient with pericarditis appears larger due to the accumulation of pericardial fluid.
- Echocardiogram. It provides an "anatomical picture of the heart and its structures, including the pericardium. If there is any change in volume, this is highlighted."
- Computed Axial Tomography (CT). Very detailed images of the heart and pericardium are obtained. It is essential to clarify the causes and to exclude pathologies other than pericarditis, but with similar symptoms. The examination uses ionizing radiation, which is slightly harmful to the patient.
- Magnetic resonance. Provides images of the pericardium and its eventual changes. The examination is not at all harmful to the patient.
Treatment
The choice of the most appropriate treatments depends on the causes and severity of the pericarditis. Therefore, a precise diagnosis is essential, which clarifies the characteristics of the disorder.
Usually, the administration of analgesic and anti-inflammatory drugs is required; surgery is rarely used, but it is indicated in cases where pericarditis is due to very serious causes (heart attack, cardiac trauma, tumors, tuberculosis, etc.).
DO YOU ALWAYS NEED HOSPITAL ADMISSION?
Whether or not to admit a patient with pericarditis is a decision for the doctor. The latter, after verifying the health conditions of the sick individual, and based on the diagnosis made, will decide what to do.
Conditions that require hospitalization:
- High fever, above 38 degrees
- High number of white blood cells in the blood, as a result of a severe infection
- Pericarditis caused by chest trauma
- High levels of troponin in the blood (N.B: troponin is a protein found mainly in voluntary muscles and in the heart. When there is muscle damage to the heart, the concentration of troponin in the blood increases abnormally)
- Risk of cardiac tamponade
- Pericarditis requiring surgery
THE PHARMACOLOGICAL TREATMENT
It is essential to know why pericarditis has arisen, as this allows the doctor to determine which medications are most appropriate. For example, viral pericarditis requires medications other than bacterial pericarditis; or, if the origin is a heart attack, some pharmacological treatments must be excluded, because they could worsen the patient's health conditions.
In summary, therefore, the most used drugs are:
- NSAIDs (non-steroidal anti-inflammatory drugs), including aspirin, ibuprofen etc.
- Narcotic analgesics
- Colchicine
- Corticosteroids
- Antibiotics
NSAIDs
Treatment with NSAIDs serves to reduce inflammation and relieve chest pain. Therefore, in addition to an anti-inflammatory action, they are also administered as analgesics.
The most used drugs are ibuprofen and aspirin. The first is very effective in almost all circumstances of pericarditis, except in cases where the origin of the disorder is a heart attack. In such situations, aspirin is used and excellent results are obtained.
The side effects, due to prolonged use, consist of gastric (stomach) ulcers. For this reason, very often, the so-called proton pump inhibitors, which protect the stomach, are associated with NSAIDs.
NSAIDs are also used in cases of recurrent pericarditis and chronic exudative pericarditis, with mixed results.
NARCOTIC ANALGESICS
By narcotic analgesics, we mean opiates (derivatives of morphine). They have excellent effects, however they should be administered for short periods and only when strictly necessary.
COLCHICINE
Colchicine performs an anti-inflammatory function, as it targets the cells of the immune system, which cause inflammation. Its administration can be associated with NSAIDs, if these have benefits, or isolated.
The action of colchicine, at the pericardial level, is effective: it reduces the symptoms and the risk of a relapse. However, in some cases, side effects may occur, such as abdominal pain, vomiting and diarrhea. , these side effects can be significantly reduced.
Colchicine effectively prevents the onset of recurrent pericarditis.
Side effects of corticosteroids:
- Recurrent pericarditis
- Weight gain
- Mood swings
- Excessive sweating
CORTICOSTEROIDS
Corticosteroids are used only when NSAID and colchicine treatments do not provide any satisfactory results. This is an extreme measure, as these drugs, especially in prolonged treatments, can have serious side effects.
Corticosteroids act on the immune system, reducing the number of inflammatory cells and, consequently, also the pain.
For further information: Drugs for the Treatment of Pericarditis "
OTHER THERAPEUTIC MEASURES
If it is ascertained that pericarditis has a bacterial origin, the therapeutic treatment involves the use, in addition to the aforementioned analgesic drugs, of antibiotics.
If the "origin of the disorder" is a heart problem, such as myocarditis or even more a heart attack, rest should be added to the appropriate drug therapy.
SURGERY: HOW AND WHEN TO INTERVENE
The surgical operation is reserved for the most severe cases of pericarditis, characterized by complications.
There are two methods of intervention and the choice of one or the other depends on the type of complications that have arisen in the patient.
- Pericardiectomy. It is the removal of the pericardium. It is used when the patient has developed chronic constricting pericarditis. In these subjects, the pericardium has become rigid as a result of the continuous inflammatory state and no longer allows the heart to pump blood normally. It is a rather delicate operation, which in one case out of 20 can lead to the death of the patient. Therefore, we only intervene if strictly necessary. Hospitalization is foreseen.
- The pericardiocentesis. It is the aspiration of pericardial fluid, when this is in excess due to the inflammatory state. The presence of too much fluid between the two layers of pericardium prevents the heart from functioning properly and pushing the blood around (as happens in cases of pericarditis chronic exudative and / or cardiac tamponade). To aspirate the fluid, a sterile, needle-like catheter is used, which is conducted to the pericardium. Drainage is repeated for several consecutive days, therefore requiring hospitalization. All this is done under local anesthesia.
Prognosis
The prognosis for pericarditis depends on the clinical case under examination. As we have seen, in fact, the inflammation of the pericardium can have different causes and, on the basis of these, more or less serious pathological circumstances will arise.
For example, viral pericarditis usually resolves positively within a few weeks, especially if the right drug treatments are applied.
Conversely, pericarditis due to some more serious heart disease, such as myocarditis or heart attack, does not have as good a prognosis as the previous case. It requires more attention and there is a risk that the disorder will recur later in time.
A condition of recurrent or even chronic pericarditis greatly affects the quality of life of an individual.
The surgery, although reserved for the most severe cases, is delicate and presents a small percentage of risk for the patient.