Generality
Cardioversion is the therapeutic procedure implemented to restore sinus rhythm in a person suffering from arrhythmia.

There is an electrical cardioversion and a pharmacological cardioversion. The first uses an instrument, the defibrillator, which emits electrical discharges; the second, on the other hand, consists in the administration of certain medicines, antiarrhythmics.
The results of cardioversion are usually more than satisfactory; however, to obtain lasting effects, it is good to follow the maintenance therapy, prescribed by the doctor, and to adopt a healthy lifestyle.
What is cardioversion?
Cardioversion is a therapeutic procedure that serves to restore the normal rhythm of the heart (sinus rhythm) in all those people who suffer from a "cardiac arrhythmia."
There are two types of cardioversion, electrical and pharmacological.
Electrical cardioversion uses electrical discharges (or shocks), generated by an instrument (the defibrillator) and transmitted to the patient through electrodes applied to the chest.
Pharmacological cardioversion, on the other hand, involves the administration of specific antiarrhythmic drugs.
Cardioversion is usually a scheduled treatment, which takes place in a hospital, but without hospitalization. In fact, at the end of the therapy, if all went well, the patient can already return home.
DIFFERENCE BETWEEN CARDIOVERSION AND DEFIBRILLATION
Defibrillation and electrical cardioversion, although based on the same operating principle, have substantial differences, so it is not strictly correct to consider them the same thing.
Defibrillation is a medical procedure practiced especially in emergencies, where the patient's life is in grave danger. Such situations are, for example, ventricular fibrillation or pulseless ventricular tachycardia, which arise and evolve very rapidly until causing the heart to stop (cardiac arrest).
Defibrillation, therefore, is not a planned intervention, as is cardioversion.
Also from the point of view of electrical discharges there is a difference: the shocks, in fact, are much stronger than those of electrical cardioversion, as the energy transmitted serves to restart the heart, not to fix its rhythm.
When you do
Cardioversion can be implemented in all those situations in which the heart beats faster (tachycardia) or irregularly (fibrillation and flutter), compared to the normal sinus rhythm.
The forms of arrhythmia for which cardioversion is ideal are supraventricular tachycardias (paroxysmal and non-paroxysmal), atrial fibrillation, atrial flutter and ventricular tachycardia with pulse; these, unlike ventricular fibrillation and pulseless ventricular tachycardia (the most suitable treatment for which is defibrillation), are less serious and more easily resolved circumstances.

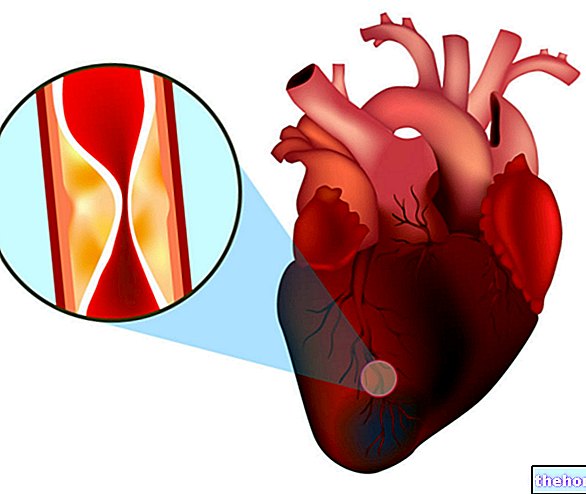
Figure: atrial fibrillation is an arrhythmia that requires cardioversion.
Not surprisingly, the procedure is often planned in advance and, before putting it into practice, the cardiologist has the time to perform a series of clinical tests on the patient.
CHOICE OF THE TYPE OF CARDIOVERSION
The choice of the type of cardioversion (pharmacological or electrical) depends on the patient's condition and on the assessments of the cardiologist.
If, once these considerations have been concluded, the practice of one or the other is indifferent, the patient can opt for the one he deems least troublesome: usually, in these cases, there is a preference for pharmacological cardioversion, since they fear electrical discharges.
Risks of the intervention
If the cardiologist takes all the necessary precautions, the risk of cardioversion producing complications is very rare.
The possible problems consist of:
- Detachment of a blood clot. It is quite frequent that those suffering from arrhythmia (especially atrial fibrillation and atrial flutter) also present one or more blood clots inside the heart. This or these clots, after cardioversion, could detach from their site and, being carried away by the blood circulation , reach various parts of the body, with sometimes dramatic results (embolism). A classic example of this eventuality is represented by a stroke, caused by a blood clot that has reached the brain. To prevent this, the patient is made to take various anticoagulant drugs for a few weeks, in order to "dilute the blood" and "dissolve" the clots present.
- Abnormal heart rhythm. It may happen that, after cardioversion, the heart rhythm, instead of returning to normal, develops another anomaly. If all this happens, the treatment must be repeated, adapting it to the characteristics of the new disorders that have arisen.
- Low blood pressure. It is possible that after cardioversion the patient may experience episodes of low blood pressure, which however improve within a few days and without any treatment.
- Skin burns. This is a drawback of electrical cardioversion; the burns are due to the electrodes, which, when applied to the chest, transmit the electric discharge.
Preparation
Before cardioversion surgery, there are some diagnostic tests to undergo, and certain precautions to take.
The diagnostic tests. The most important is, undoubtedly, the so-called transesophageal echocardiogram, which is carried out to "find" any blood clots inside the heart. The examination procedure involves the use of an ultrasound probe, which, when applied to a " end of a flexible tube (a catheter), is inserted into the mouth and lowered to the esophagus. Once positioned in the appropriate place, the probe projects, on a monitor, clear images of the heart and its internal anatomy.
In addition to the transesophageal echocardiogram, all those routine pre-surgery diagnostic tests (blood pressure analysis, blood tests, etc.) are then performed.
Pre-intervention precautions. Before the procedure, it is necessary to refrain from eating and drinking for at least 6/12 hours, as general anesthesia is required. If the patient is taking any medications, it is advisable to report it to the doctor and ask for advice on what to do.
Frequently Asked Questions About Transesophageal Echocardiography
How long does it last?
The duration is about 20-25 minutes.
Is it painful?
The patient may feel pain as the catheter is passed through the mouth and esophagus. This is a tolerable sensation that can be prevented with light sedation.
Do I need to fast before the exam?
Yes, you must have been fasting for at least 6/12 hours.
Do you need hospitalization?
No, however it is advisable to be accompanied by some family member (or friend) because the anesthetic, used for sedation, can alter the driving skills of the patient.
WHAT TO DO IF THERE ARE BLOOD CLOTS IN THE HEART?
If, from the transesophageal echocardiogram, the presence of one or more clots emerges, the cardiologist prescribes to the patient anticoagulant drugs, to dilute the blood. The treatment, for it to take effect, must last for at least four weeks. Only once this cure is done. anticoagulant is considered finished, cardioversion can be practiced.
The most commonly used anticoagulant is Coumadin.
Procedure - Electrical cardioversion
Electrical cardioversion requires general anesthesia to sedate the patient.
Electric shocks are emitted by an instrument, called a defibrillator, which is connected to the patient via electrodes, applied to the chest (or even to the back).

Figure: instrumentation for electrical cardioversion. The electrodes are the two plates visible in the photo.
The defibrillator is an "intelligent" device, because it is able to record the heart rhythm of the patient and notify the cardiologist when "is the most suitable time to release the shock.
The intensity of the shocks is at the discretion of the physician and depends on the ailment afflicting the patient.
SEDATION
General anesthesia involves the use of anesthetics and pain relievers, which make the patient unconscious and insensitive to pain.
The administration of these drugs, carried out intravenously, occurs before and for the duration of the procedure.
In fact, once the cardioversion is completed, the pharmacological treatment is stopped to allow the patient to regain consciousness.
Some anesthetics (for example, lidocaine) have a dual function, analgesic and antiarrhythmic. Therefore, they are administered with a dual purpose: to anesthetize the patient and facilitate the resumption of normal cardiac activity.
PATIENT MONITORING
To see how a patient's heart responds to electrical shocks, a continuous electrocardiogram is used. Only in this way, in fact, is the cardiologist able to know how the situation evolves after each shock and, possibly, if he has to make changes to the intensity of current emitted by the defibrillator.

Figure: an electrocardiographic trace. It can be seen how the electrical discharge (shock) restores the normal heart rhythm, previously altered by atrial fibrillation.
DURATION
Once the patient is sedated, electrical cardioversion takes place within minutes. The duration varies from patient to patient and depends on how long and how many shocks it takes to restore sinus rhythm.
AFTER THE INTERVENTION
Electrical cardioversion is an outpatient type procedure, which takes less than a day and does not require any hospitalization.
Before discharging the patient, however, it is advisable to keep him under observation for at least an hour; this is a normal precautionary measure, in the event that complications should arise.
The key points of the post-intervention phase are:
- Assistance of a family member. It is important to remember that general anesthesia may reduce the ability to sense and, in general, attention. For this reason, it is good to be driven home by a family member or friend, as it is strongly not recommended to drive a vehicle immediately.
- Anticoagulant drugs. Even if the heart, before the surgery, did not have blood clots inside it, anticoagulants are still prescribed for preventive purposes.
- Maintenance therapy. Also for preventive purposes and to consolidate the effects of electrical cardioversion, the patient is prescribed a treatment based on antiarrhythmic drugs. If well tolerated by the patient, this therapy can last a lifetime. Any decision regarding the dosage or the interruption of treatment is the sole and exclusive responsibility of the physician.
Procedure - Pharmacological Cardioversion
Pharmacological cardioversion involves the administration of antiarrhythmic drugs, intravenously or orally.
The antiarrhythmics available are divided into 4 classes, based on the mechanism of action:
- Sodium channel blockers (class I): by exerting a blocking action on the so-called sodium channels, stabilizing the heart rhythm. There are three different subclasses: IA, IB and IC (see the following table).
Class I antiarrhythmics or sodium channel blockers
IA
IB
IC
Procainamide
Quinidine
Disopyramide
Lidocaine
Phenytoin
Mexiletine
Propafenone
Flecainide
Moricizina
- Cardioselective beta-blockers (Class II): slow the heart rate by specifically blocking the beta-1 adrenergic receptors acting on the heart. By the term cardioselective, they are distinguished from beta-blockers of beta-2 receptors, which have effects on the bronchi and blood vessels.
- Potassium channel blockers (Class III): restore normal heart rhythm by blocking potassium channels. In cases of atrial fibrillation and atrial flutter, azimilide and ibutilide are widely used; in cases of paroxysmal supraventricular arrhythmias, sotalol is usually administered; in many tachycardias, amiodarone is used.
- Calcium channel blockers (Class IV): slow down the heart rate and regulate it by blocking the calcium channels. The most commonly used are diltiazem and verapamil.
(class IV):
Metoprolol
Atenolol
Acebutolol
Azimilide
Ibutilide
Sotalol
Amiodarone
Diltiazem
Verapamil
AFTER THE ADMINISTRATION OF THE ANTIARRITHMIC
After drug administration, the patient undergoes an electrocardiogram (as in electrical cardioversion), to see what the response to treatment is.
If everything goes smoothly, the doctor plans the most appropriate maintenance therapy.
The latter is based on antiarrhythmics and serves to keep the heart rhythm within the desired values.
DURATION
Pharmacological cardioversion itself is very short. Once the drug has been taken, in fact, it can be considered finished.
MAINTENANCE THERAPY
Maintenance therapy, if well tolerated by the patient, can also last a lifetime.
On the other hand, should any disorders related to the continuous intake of antiarrhythmics occur, the treatment must be interrupted, observing what are the subsequent reactions of the patient.
In these situations, every decision rests with the cardiologist, who also decides how and whether to replace maintenance therapy.
Results
In most cases, cardioversion (both electrical and pharmacological) restores normal heart rhythm.
When it does not have the desired success (usually, the disorders reappear after a few hours or days), the only solution is to repeat the procedure, perhaps adjusting the power of the electric shock or the drug dose.
HOW TO PREVENT RELAPSE?
A healthy lifestyle and some health measures help prevent arrhythmias, especially in people who are predisposed to these heart conditions or who have already suffered from it in the past.
Here are some important medical tips:
- Eat healthy foods and maintain a normal body weight
- Reduce the salt taken in the diet, so as not to raise blood pressure
- Exercise (commensurate with your possibilities)
- Limit or avoid caffeine intake
- Not smoking
- Limit or avoid alcohol altogether
- Keep cholesterol levels low
- Reduce stressful situations
- Be careful with each medicine you take, as it may alter the heart rhythm stabilized by cardioversion.










-nelle-carni-di-maiale.jpg)