In a fair number of cases, Brugada syndrome is due to a genetic mutation; more often, however, it has an "origin that doctors still cannot explain.
This heart disorder is difficult to diagnose: in fact, a particular electrocardiographic examination is often needed to identify it.
There is no cure for Brugada syndrome; however, the consequences can be controlled with an implantable defibrillator.
What are Cardiac Arrhythmias: a brief review
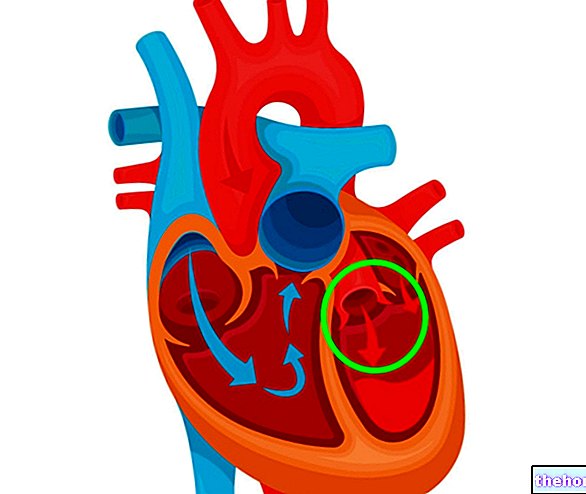
The human heart is made up of four muscular compartments (the two atria and the two ventricles), which contract synchronously and with a certain cadence in order to ensure the correct blood supply of the various organs.
To ensure the correct contraction of the heart - more precisely of the myocardium, the heart muscle - are electrical impulses generated by some specific areas of the same muscle tissue.
When something alters the generation of the electrical impulses necessary for the correct contraction of the heart, it is in the presence of a "cardiac arrhythmia."
, more precisely of the electrical activity of the heart, which can cause severe, sometimes even fatal, episodes of ventricular arrhythmia.
Brugada syndrome is known to be a leading cause of sudden cardiac death.
For further information: Sudden Cardiac Death: What is it?Epidemiology: how common is Brugada syndrome
Brugada syndrome is a rare condition: according to reliable estimates, in fact, 1 to 30 people per 10,000 individuals considered would be affected.
Although it is a congenital disorder, Brugada syndrome emerges mainly in adulthood (30-40 years), while it is rare to observe its consequences at a young age (although not impossible).
Among adults, the condition is more often symptomatic for men than for women; this difference, however, is not observed in young people, for whom the disease is symptomatic in both sexes in equal measure.
Brugada syndrome is more common among populations of Asian origin, in particular among people originating from Thailand and Laos.
According to reports from the medical literature, Brugada syndrome is the cause of 4-12% of all cases of sudden cardiac death and more than 20% of all cases of sudden cardiac death in people with a structurally healthy heart. .
Brugada syndrome: origin of the name
Brugada syndrome owes its name to two brothers of Spanish origin, Pedro and Josep Brugada, both cardiologists, who had the merit of describing it accurately in 1992.
It should be noted, however, that the discovery of the Brugada syndrome dates back to a few years earlier, exactly in 1988, when a group of Italian researchers outlined its main features in the Italian Journal of Cardiology.
Brugada Syndrome: Synonyms
Brugada syndrome is also called Nava-Martini-Thiene syndrome, in honor of the Italian researchers who in the 1980s outlined the characteristics of the condition.
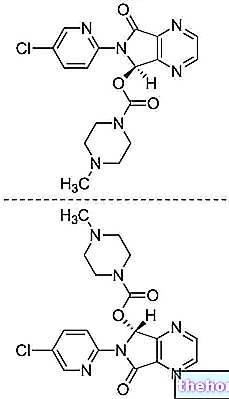
of heart cells, a behavior that produces an "alteration of the ionic currents that cross the aforementioned membrane and that regulate the electrical impulses mentioned above.
Brugada Syndrome: What Are the Causes?

In 30-35% of cases, the cause of Brugada syndrome is an inherited genetic mutation, involving a gene encoding a membrane channel present primarily in heart muscle cells or a protein connected to that channel.
In the remaining percentage of cases (therefore 65-70%), however, the cause of the condition in question is not (yet) attributable to a specific factor, be it genetic or otherwise.
For obvious reasons, the first of the two situations is the best known and for which there are more studies.
Brugada syndrome: the responsible genes
Currently, researchers have identified at least 18 genes whose mutation would play a role in the onset of the genetic and heritable form of Brugada syndrome.
Among these genes, SCN5A stands out in particular, as it is implicated in a percentage of cases of Brugada syndrome that varies between 10 and 30%.
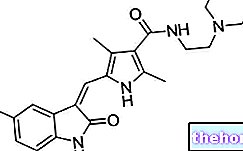
Located on chromosome 3, SCN5A encodes the alpha subunit of a voltage-dependent sodium channel found primarily in cardiac cells, whose task, when normal (i.e. not mutated), is to contribute to the transmission of electrical signals responsible for the correct contraction of the myocardium.
Other genes that research has identified as potential responsible for Brugada syndrome are: SCN1B, SCN2B, SCN3B, SCN10A, ABCC9, GPD1L, CACNA1C, CACNB2, CACNA2D1, KCND3, KCNE3, KCNE1L -KCNE5-, KCNJANGR, HCNJ8 and TRPM4.
When mutated, the SCN5A gene produces a defective channel, which impairs the correct transmission of the electrical signals necessary for cardiac contraction.
Brugada Syndrome and Heredity
Genetically based Brugada syndrome is a hereditary condition, that is, it can be transmitted from parents to children.
The transmission pattern of this disorder is, in most cases, of the autosomal dominant type; this means that, in order to suffer from the disease, it is sufficient for parents to pass on a single copy of a gene potentially responsible for the condition.
"Autosomal" means that the gene involved in the disease resides on a non-sex chromosome.
"Dominant", on the other hand, refers to the fact that the copy of the mutated gene, as it is altered, dominates the effects of the copy of the normal gene.
It should be added that, for inheritable genetic diseases with autosomal dominant transmission, it is sufficient for a single parent to present a copy of the mutated gene for the child to develop the disease.
Brugada Syndrome: Risk Factors
Factors favoring Brugada syndrome include:
- Inheritance and family history. The children of a person with Brugada syndrome present, despite themselves, a good chance of being affected by the same heart disorder; this is because, as noted above, the condition is not infrequently connected to inheritable genetic mutations.
- The male sex. In people who carry it, Brugada syndrome tends to occur more frequently in men than in women; this is probably due to hormonal reasons.
- Belonging to the Asian population. Among Asians, particularly those coming from Thailand and Laos, Brugada syndrome is more common than in other populations.
When the disease presents with symptoms, the latter are the consequence of a ventricular arrhythmia (ventricular fibrillation or polymorphic ventricular tachycardia) and could consist of:
- Fainting (or syncope)
- Palpitations;
- Difficulty in breathing (dyspnoea);
- Chest pain;
- Dizziness;
- Convulsions;
- Cardiac arrest.
How Brugada syndrome might manifest varies from patient to patient; in other words, the aforementioned disorder does not lead to cardiac arrest for all patients, but is limited to less severe symptoms.
There is, however, a common aspect to report regarding the symptoms: generally, people with Brugada syndrome manifest the condition during the night or after a heavy meal (less frequently at rest).
For further information: Brugada Syndrome: all the SymptomsSign of Brugada: What is it?
As will be seen in the chapter dedicated to diagnosis, carriers of Brugada syndrome show a particular electrocardiographic trace (ECG), known as Brugada's sign, whose presence is not associated with obvious symptoms or disorders (in simpler words, patients manifest an "anomaly in the electrocardiographic tracing, without however complaining of related disturbances).
It is important to note that all cases of Brugada syndrome have the homonymous sign, but not all those who appear to have this sign are carriers of Brugada syndrome.
This makes it essential to investigate the situation, through further checks, in order to understand what the actual heart problem is.
Brugada Syndrome: What Can Trigger Symptoms?
Studies regarding Brugada syndrome have shown that certain factors can unmask the condition and trigger symptoms.
These factors include:
- High fever;
- Electrolyte changes, such as hyperkalaemia, hypokalaemia or hypercalcemia;
- Excessive consumption of alcoholic substances;
- Use of cocaine;
- Drugs, such as beta-blockers, drugs with vagotonic effect, class I antiarrhythmics that block sodium channels, alpha-adrenergic agonists, heterocyclic antidepressants.
Brugada Syndrome: Complications
As anticipated in part, Brugada syndrome can cause sudden cardiac death as a result of cardiac arrest.
Cardiac arrest represents a medical emergency that requires immediate therapeutic intervention in order to save the patient's life.
Did you know that ...
Sudden cardiac death from Brugada syndrome occurs mostly during the night while the patient is asleep.
Brugada syndrome: when to see a doctor?
Those suffering from sudden palpitations, breathing difficulties, chest pain and fainting should contact their doctor and undergo cardiologist checks as soon as possible, to find out the precise cause of the aforementioned problems.
In addition, people with a family history of Brugada syndrome are strongly advised to have a genetic test for the most common mutations associated with the aforementioned condition.
they can provide useful information, especially in the presence of a family history of Brugada syndrome; however, they are not sufficient to establish a definitive diagnosis.
To be sure that an individual is affected by Brugada syndrome, the electrocardiogram, the echocardiogram and the stress test are essential; in addition, the specific genetic test for the identification of the disease is also valuable and enriches with further information.
Physical examination and anamnesis
The physical examination consists in the analysis of the symptoms (if the patient had had a suspected episode which resolved for the best) and in the auscultation of the heart.
The data collected on that occasion are insufficient to establish a diagnosis, due to the very characteristics of Brugada syndrome and the fact that many other conditions cause similar symptoms.
The physical examination, however, can acquire considerable value if a family history of Brugada syndrome or sudden cardiac death emerges from the following medical history (eg: a parent suffering from Brugada syndrome or who died of an episode of sudden cardiac death ).
Electrocardiogram

The electrocardiogram (ECG) is the examination of choice for the identification of the sign of Brugada and the homonymous syndrome.
However, it should be noted that the diagnosis of Brugada syndrome by ECG is not always immediate; this is because the disorder is extremely variable over time and at the time of examination it could be in a phase of complete latency, such that the ECG does not show any suspicious signs.
To overcome this problem, the cardiologist on duty could, in the meantime, resort to a 24-hour ECG holter and, subsequently, if there are still strong doubts, the so-called test with flecainide or ajmaline, a very specific examination capable of bringing out the diagnostic electrocardiographic profile for Brugada syndrome.
Characteristics of the Sign of Brugada
Brugada's sign is characterized by an elevation of the ST segment in any of the right precordial leads (V1-V3) with a right branch block.
This is, in reality, a simplification of the Brugada sign: there are, in fact, several variants of the same, however, to understand them, very specific knowledge of cardiology would be needed.
Test with Flecainide or Ajmaline
Performed in day hospital, the test with flecainide or ajmaline involves the administration of one of these two drugs, followed by an electrocardiogram.
Flecainide and ajmaline are two class 1A antiarrhythmic drugs with blocking properties against the sodium channel, capable, in people with Brugada syndrome, to bring out the diagnostic electrocardiographic profile for the disease.
Echocardiogram
The "echocardiogram is, essentially, an" ultrasound of the heart; it, therefore, provides images related to its anatomy, from the heart chambers (atria and ventricles) to the heart valves etc.
The "echocardiogram does not allow the diagnosis of Brugada syndrome; however, it is still useful, because it allows the doctor to exclude the possibility that the symptoms complained of by the patient and / or any abnormal electrocardiographic trace (*) are due to causes other than the aforementioned heart disease (e.g. valvulopathy, ventricular hypertrophy, etc.).
(*) N.B: remember that, despite the name, the Brugada sign is also observable in the presence of other cardiac disorders.
Genetic Test
Genetic testing is recommended for all patients with a family history of Brugada syndrome.
It allows to identify the genetic mutations associated with heart disease, confirming what emerged from a possible ECG or from other clinical investigations.
However, it should be noted that, in the presence of suspicious symptoms, diagnostic investigations cannot be limited to genetic testing: readers are reminded, in fact, that Brugada syndrome is connected to a heritable genetic mutation only in 30-35% of cases.
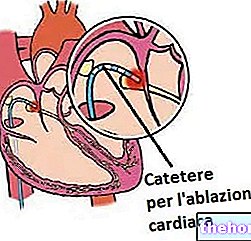
introduced into the heart, the myocardial area responsible for the incorrect transmission of electrical signals.Radiofrequency catheter ablation is an extreme treatment, adopted only in those patients for whom the ICD has proved ineffective or dangerous.
Brugada Syndrome: What to Avoid to Reduce the Risk of Arrhythmias
Various behaviors help reduce the risk of Brugada syndrome triggering a "ventricular arrhythmia, with all the consequences of the case; these behaviors include:
- Immediately treat febrile states with appropriate antipyretic drugs. As previously stated, the increase in body temperature favors the appearance of the typical symptoms of Brugada syndrome.
- Avoid taking drugs capable of altering heart rhythm. Some of these drugs are beta-blockers, sodium channel blocking class I antiarrhythmics, tricyclic antidepressants, alpha-adrenergic agonists and drugs with a vagotonic effect.
- Avoid excessive alcohol consumption.
- Avoid the consumption of cocaine and other related drugs.
- Avoid practicing sporting activities at a competitive level.













-nelle-carni-di-maiale.jpg)