For this reason, when an altered fasting glucose is detected, we often speak of prediabetes, a yellow light that should invite the patient to pay greater attention to nutrition and the level of daily physical activity.
.jpg)
Altered fasting blood glucose is a warning that reminds us of two very important things. The first is that type II diabetes mellitus does not strike suddenly, but in most cases, if not always, it passes through a reversible condition and not exactly pathological that lasts for years. This condition, which we can identify in the "altered fasting glycaemia, does not give particular symptoms, which is why after the forty-fifth birthday, especially in the presence of overweight and familiarity with the disease, it is necessary to monitor one's blood sugar with some attention. assessment is negative, the test must be repeated after three years.
For the high-risk population (pre-diabetic states, family history of diabetes mellitus, metabolic syndrome, hypertension, hyperlipidemia, mothers of macrosomic newborns), on the other hand, diagnostic investigations should be considered earlier and performed at least annually. .
Although they are not real diseases, the finding of pre-diabetic states should never be underestimated, as they represent an important risk factor for the future development of overt diabetes, as well as being associated with an "increased incidence of atherosclerotic and in particular of ischemic heart disease.
(IGT), although the two conditions can coexist.
The diagnosis of IGT is made through the so-called oral glucose load, in which the patient's glycemic response to the ingestion of 75 grams of glucose dissolved in water is recorded over time; if after two hours the blood glucose levels are higher than certain threshold values (> 140 mg / dL but lower than 200 mg / dL), we speak of IGT. This condition presents a greater risk of evolution into overt diabetes than IFG and it is for this reason that after the detection of an altered fasting blood glucose very often the doctor directs the patient to an oral glucose load test.
Pre-diabetic states are represented by impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG).
Depending on the sources, we speak of impaired fasting blood glucose when the blood glucose levels measured on a small venous blood sample, taken after fasting for at least 8 hours (only water is allowed), are:
- greater than or equal to 110 mg / dL (6.1 mmol / L), but still less than 126 mg / dL (6.9 mmol / L, which are pathognomic of diabetes) - WHO Guidelines World Health Organization -
- greater than or equal to 100 mg / dL (5.6 mmol / L), but still less than 126 mg / dL (6.9 mmol / L, which are pathognomic of diabetes) - ADA guidelines American Diabetes Association.
To learn more, read: Example diet for type 2 Diabetes Mellitus
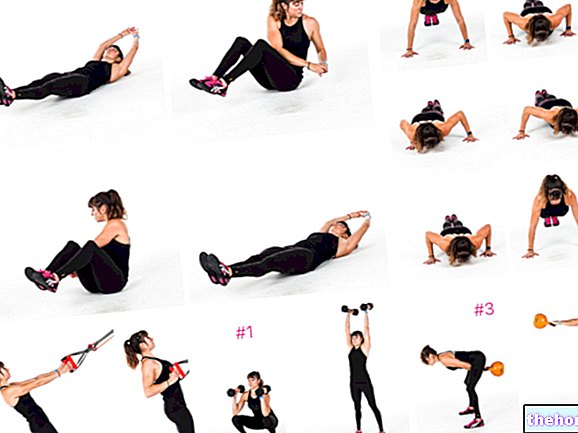
The dietary intervention will be accompanied by greater physical activity, the more important the more the person is overweight. Nobody, however, will ask you to become an athlete: walk briskly for thirty minutes a day (or at least do it 4 times per week) and preferring a few healthy flights of stairs to the lift is an extraordinarily effective strategy to prevent diabetes and improve general well-being and lipid profile (cholesterolemia, triglyceridemia, etc.).
To learn more, read: Physical activity and Type 2 diabetes