More in detail, we will give a brief overview of the generalities of the pathology, mentioning the causes, consequences and possible treatments.
Later, we will go into the details of the dedicated motor therapy, mentioning the types and methods with which to intervene in case of type 2 diabetes mellitus - even with complications.
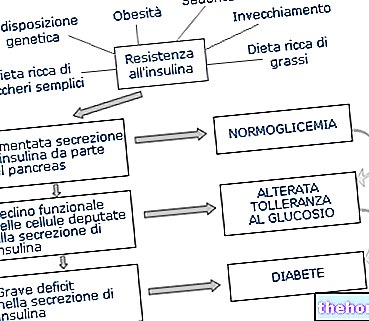
chronic (excess of glucose in plasma) based on two pathological mechanisms, co-present or not:- Insulin resistance: defect of insulin action on peripheral tissues (obviously, insulin-dependent);
- Insulin synthesis deficiency: reduced production of the hormone by the pancreas.
Note: Insulin synthesis deficiency is often a long-term complication of insulin resistance.
It occurs mainly in adults and is the most common form of diabetes (90% of cases).
Unlike type 1, it is not insulin dependent - although in severe cases, in which the pancreas stops functioning as it should, exogenous insulin therapy may still become necessary.
The causes can be of hereditary (polygenic) or environmental nature; among the latter stand out mainly: obesity, sedentary lifestyle, unbalanced diet characterized by excess carbohydrates, stress, other diseases and certain drugs.
Obesity and Diabetes
Obesity is present in more than 80% of cases of type 2 diabetes mellitus.
Adipose tissue is capable of producing a series of substances (leptin, TNF-α, free fatty acids, resistin, adiponectin) which, if in excess, contribute to the development of insulin resistance.
Furthermore, in obesity, adipose tissue is the site of a state of chronic low-intensity inflammation, which is a source of chemical mediators that aggravate insulin resistance.
Type 2 diabetes mellitus increases the danger of early death and permanent disability; it seems to increase above all cardiovascular risk and, in particular, in association with other pathological forms such as: arterial hypertension, dyslipidemia (hypercholesterolemia and hypertriglyceridemia).
In the early stage, type 2 diabetes mellitus does not always cause noticeable symptoms; on the contrary, it is almost always completely asymptomatic until the first complications arise.
Only a haematological investigation can highlight chronic hyperglycemia, the consequent compensatory hyperinsulinism and a state of excessive protein glycation. More specific analyzes, such as the load curve, will confirm the diagnosis.
However, chronic hyperglycemia can manifest itself with: tiredness, frequent urination, excessive thirst, difficulty losing weight or vice versa, unmotivated weight loss, slow wound healing, blurred vision.
Treatment of type 2 diabetes mellitus should be multidisciplinary. The importance of one aspect or the other can vary according to the subjective framework. Pharmacological use is crucial above all in restoring general homeostasis in the short term, even if food and motor therapy are the only solutions for type 2 diabetes mellitus not complicated by loss of pancreatic function.
The use of oral hypoglycemic agents is the most common strategy, while the administration of insulin is limited to cases in which the pancreas has stopped synthesizing it adequately.
In the obese, the diet is aimed above all at fat loss. It is advisable to structure it in a balanced way, keeping the carbohydrate fraction at the lower limit of the normal range. Establishing ketosis can represent a significant risk for diabetics with kidney complications.
Physical activity, on the other hand, in addition to supporting weight loss, must:
- Increase insulin sensitivity;
- Improve the management of dietary carbohydrates.
Obviously, everything will have to take into account any complications and contraindications.
both in acute, ie during practice, and in chronic, ie in the long term.Among the benefits of training on type 2 diabetes mellitus we recognize above all the increase in insulin sensitivity and an increase in the efficacy of cellular glucose transport, with a reduction in blood sugar, insulinemia, triglyceridemia and glycated proteins.
The improvement of insulin sensitivity and the emptying of hepatic and above all muscle glycogen reserves promote better management of dietary carbohydrates, helping to optimize weight loss - a factor which, in itself, increases insulin sensitivity.
Benefits on insulin sensitivity
Insulin resistance compromises the absorption of insulin-mediated glucose, therefore on insulin-dependent tissues, by 35-40% compared to healthy people.
The most abundant insulin-dependent tissue in the body is skeletal muscle, which therefore positively correlates with the ability to absorb glucose - while fat mass has an inverse correlation.
In acute cases, motor activity increases insulin sensitivity for 24-72 hours after training even in subjects with type 2 diabetes mellitus.
After this period of time, it is necessary to apply a new physical stimulus to restore this advantageous condition. This is why, especially those with type 2 diabetes mellitus, he should train more or less every other day.
Benefits on glucose transport
The metabolic use of glucose in muscle fiber cells occurs, very briefly, as follows:
- Transition from plasma to muscle tissue: physical training improves muscle blood flow, thanks to greater cardiac action and peripheral capillarization. Good spraying is crucial to meeting the need for glucose, oxygen, etc. muscles, and allows the disposal of waste residues. Acute motor exercise also promotes the opening of capillaries that are not normally used; in the chronic it stimulates a "further branching;
- Carriage of glucose across the cell membrane: the trans-cellular transport of glucose occurs through glucose transporters 4 (GLUT-4), which are normally found in the intracellular cytosol. Physical training stimulates the emergence of the latter, making the cell more able to pick up glucose;
- Phosphorylation: the energetic use of glucose occurs thanks to an enzyme called hexokinase, which significantly increases in concentration if motor activity is performed regularly over the long term.
Attention! A consistent metabolic activation, due to a relative training load, in acute and immediate post exercise, makes the muscle cells partially independent from the insulin action.
Benefits on the management of dietary carbohydrates
Motor activity makes the body better able to manage the post-prandial glycemic load.
This is due, in addition to the metabolic and functional modifications of the acute phase, also to an adequate emptying of the hepatic and muscle glycogen reserves.
This depletion increases the "greed" of these glucose tissues even away from training.
Benefits of physical activity on other risk factors
Physical exercise also affects the other risk factors for death and permanent disability, linked to atherosclerosis and cardiovascular events; we are talking about: primary arterial hypertension, dyslipidemia, obesity.
Present in over 60% of type 2 diabetics, primary arterial hypertension is the statistically most damaging and dangerous comorbidity.
They are normal blood pressure <140/90 mm Hg, borderline between 140/90 and 160/95 mm Hg and pathological when higher.
Regular physical activity lowers blood pressure levels in healthy people with type 2 diabetes, thanks to improved cardiovascular efficiency. Hypertension is also reduced as a result of weight loss and by reduction of central nervous effects.
The recommended type of training is an aerobic background, even with considerable intensity - in trained subjects. The use of weights is not contraindicated, unless the Valsalva maneuver is established or except for high intensities.
Aerobic physical exercise reduces triglyceridemia, also as a result of better glycemic management.
It also improves cholesterolemia, with an increase in HDL and a percentage reduction in LDL. Total cholesterol does not always decrease. Consequently, the risk of atherosclerosis and coronary heart disease is also lowered.
Physical activity promotes weight loss only when associated with controlled (hypocaloric) dietary therapy. Vice versa, in the measure of about 20-30 minutes a day at moderate intensity, it has more than anything else a "preventive action on" increase.
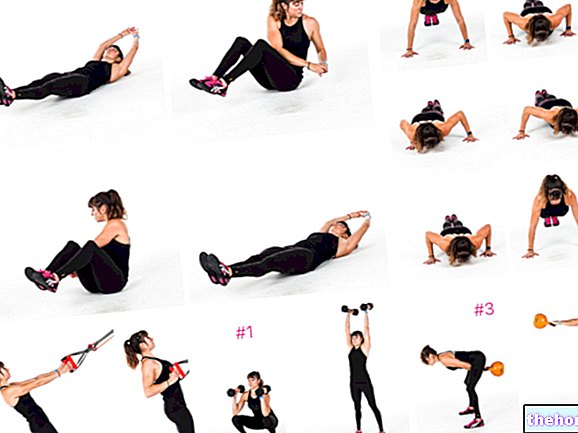
and obese. It too improves insulin sensitivity, increases calorie expenditure and optimizes the quality of life; it also increases muscle strength, lean mass and bone mineral density.The right training load is at least 2-3 days a week, with 8-10 exercises targeting the largest muscle groups, for 1-3 sets of 10-15 repetitions each. The "intensity" must be increasing, and in any case not less than 50% of 1RM.
they are allowed, however it is necessary to pay attention to those already dangerous in themselves or for which a "hypoglycemia could induce serious consequences.
It is advisable to choose mainly aerobic alactacid physical activities, without forgetting that the achievement of high intensities correlates with an improvement of various functional and metabolic parameters (cardio-circulatory and respiratory efficiency, etc.).
By also combining resistance training, it will be possible to take advantage of the benefits that low intensity aerobic activity does not by itself confer.
Also the aspect of flexibility, elasticity and joint mobility should not be overlooked. This type of training significantly reduces the risk of injury and improves the general quality of life, but does not bring metabolic benefits.
Frequency
The frequency of recommended physical activity varies from 3 to 5 sessions per week, avoiding periods of inactivity for more than 2 days in a row - for the reasons we have explained above.
Duration
No less than 20-30 "and up to 60" of activity per workout are recommended, plus 5-10 minutes of warm-up and 5-10 minutes of cool-down - also for flexibility, elasticity and mobility protocols.
Intensity
Aerobic activity should be low initially and then moderate intensity (40-60% of VO2max or 50-70% of HR max) for a total of 150-200 "per week.
By increasing with intensity (> 60% of VO2max or> 70% of Fcmax), it is possible to reduce the volume to 90 "weekly.
Precautions
Before starting a physical activity program, the patient should be aware of the precautions to be taken before, during and after the activity.
Glycemic control is the fundamental element to check before starting, but also during (if the activity lasts over time) and after physical activity.
The guidelines, in fact, advise to avoid undertaking the activity if the glycaemia is> 250 mg / dl or if ketonuria is present.
However, it should be noted that a "light or moderate intensity may be useful in" lowering acute glycemic levels.
Attention should also be paid to the combination of motor activity and drug therapy. Often, improved metabolic fitness makes treatments excessively hypoglycemic.
Be careful to keep the state of hydration high.
Physical activity guidelines in the presence of complications
The physical activity protocol for subjects with complications must be adapted according to the same; in particular: ischemic heart disease, diabetic nephropathy, retinopathy, sensory-motor neuropathy and autonomic neuropathy.
Ischemic heart disease
Physical activities that produce precordial pain or a strong increase in heart rate should be avoided, while it is recommended to practice physical activities of low-moderate intensity (40% of Vo2max or 50% of HR max).
Diabetic nephropathy
Only moderate-intensity physical exercises (walking, swimming, biking) are recommended.
Diabetic retinopathy
Physical activities that involve an increase in blood pressure (such as high-intensity weightlifting and with Valsalva) or that involve physical contact (such as combat sports) should be avoided, while moderate-intensity physical activities are allowed.
Sensory-motor neuropathy
Regular practice of alactacid aerobic exercise can slow the progression of peripheral neuropathy, but for the potential traumatic effects on the feet, only weightless exercises (stationary biking, rowing, swimming) are recommended.
Autonomic neuropathy
Light physical exercises and aerobic activities are allowed in suitable temperature conditions, with adequate hydration.

.jpg)