Generality
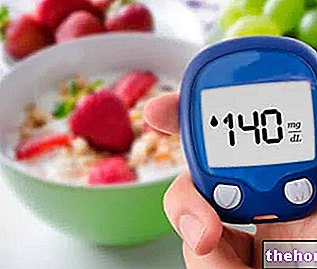
Postprandial blood glucose is a numerical value that indicates how much glucose is present in the blood two hours after the end of a meal.
After 60-120 minutes from the conclusion of a substantial meal (abundant breakfast, lunch or dinner), the glycemic levels record the maximum peaks of the day. This phenomenon, absolutely normal within certain limits, is linked to the entry into the circulation of glucose deriving from the digestion of carbohydrates and absorbed in the intestine.
Postprandial glycaemia is controlled by insulin secreted by the pancreas, in order to favor the entry of blood glucose into cells, which use it for energy purposes or transform it - especially in the liver - into metabolic reserve (in the form of glycogen and / or triglycerides).
Thus, in healthy people, postprandial glycemic levels rarely rise above 140 mg / dl (7.8 mmol / l), and then return to baseline levels within 3-5 hours of food ingestion.
Postprandial hypoglycemia, in-depth article.
Health hazards
In people with overt diabetes or in a state of impaired glucose tolerance (IGT), the mechanism just described does not work properly. Consequently, postprandial glycaemia rises above the levels considered normal, bordering on the pathological.
Over time, the recurrence of postprandial hyperglycemic phenomena ends up damaging the eyes, kidneys, nerves and blood vessels. In particular, a "high postprandial glycaemia is related to the development of complications of diabetes, both type one and second type. Among the most serious are neuropathy, renal insufficiency, vision loss, macrovascular diseases and amputations. Up to a few years ago, the prevention of these complications, and the therapy of diabetes itself, mainly focused on the reduction of HbA1c levels (glycated hemoglobin) and on the control of fasting plasma glucose. Today, however, the treatment is also aimed at reducing of postprandial glycemic excursions, considered equally important - if not even more important - for the achievement of optimal glycemic control and for the prevention of complications, especially of a macrovascular nature. The latter are responsible for the net increase in mortality from diseases such as myocardial infarction and stroke compared to the healthy population.
The World Health Organization defines normal glucose tolerance as glycemic values below 140 mg / dl (7.8 mmol / l) two hours after ingestion of a 75 g glucose load, in the context of an oral test of glucose tolerance. In these guidelines, postprandial hyperglycemia is defined as levels above 140 mg / dL (7.8 mmol / L) two hours after food ingestion.
Postprandial hyperglycemia begins before type 2 diabetes, when the patient is still in a pre-diabetic state, defined as impaired glucose tolerance.
How is it measured?

Treatment
What to do to decrease postprandial blood glucose levels
Nutritional interventions, physical activity and body weight control are the cornerstones of effective diabetes management, including from a preventive perspective.
As stated in the previous chapter, the purpose of these interventions - possibly assisted by specific pharmacological therapies - is to achieve optimal glycemic levels, not only in fasting conditions (<100 mg / dl or 5.5 mmol / l) but also in the post- meal (<140 mg / dl or 7.8 mmol / l).
Low glycemic index (GI) diets are beneficial in postmeal plasma glucose control. These dietary strategies are based on the prevalent consumption of foods rich in fiber (vegetables, legumes and unsweetened fruit), as opposed to the moderation of foods rich in complex carbohydrates (pasta al dente, rice, wholemeal bread, baked goods and cereals in general, potatoes, tubers, chestnuts) and the avoidance of simple sugars (sucrose, white bread, honey, sweets, snacks, sugary drinks, etc.). In the "practical application of the glycemic index, however, the concept of glycemic load should not be forgotten, given from the product between the carbohydrate content of the diet and its average GI, it is therefore necessary to focus both on the choice of carbohydrates with the lowest glycemic index and on their quantitative moderation.
Various pharmacological agents preferentially reduce postprandial plasma glucose.This category includes inhibitors of "α-glucosidase (acarbose), glinides (fast-acting insulin secretagogues) and of course" insulin (fast-acting insulin analogues, biphasic [premixed] insulins, inhalation insulin, insulin regular human). In addition, new therapeutic classes for the treatment of postprandial plasma glucose in diabetic patients - among which we recall the analogues of amylin, derivatives of glucagon-like peptide-1 [GLP-1] and inhibitors of dipeptidyl peptidase-4 [DPP -4] - have been shown to bring significant benefits in reducing glycemic excursions after meals. These therapies control fasting and postprandial glycaemia by acting on the deficiency of pancreatic and intestinal hormones, which affect the secretion of insulin and glucagon, the sensation of satiety and gastric emptying.