Generality
Gestational diabetes (GDM) is a metabolic disorder characterized by impaired glucose tolerance (and less frequently frank diabetes), which arises or is first diagnosed during pregnancy.

Causes
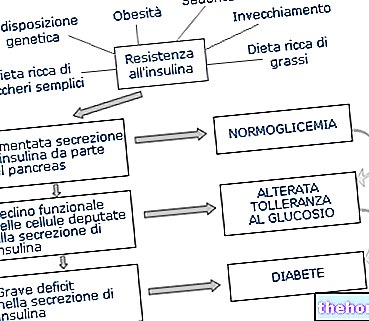
The hormonal upsets related to pregnancy increase the resistance to insulin, making the cells less sensitive to its action. The pancreas, for its part, is not always able to compensate for this deficit through a proportional increase in the synthesis and release of insulin.
Gestational diabetes is therefore a phenomenon in certain aspects "physiological", which as such does not normally involve serious dangers for the mother and the unborn child. In fact, it is well known that the period most at risk of congenital fetal malformations is the one between conception and the tenth week of pregnancy, while gestational diabetes tends classically to occur after the twenty-fourth week, when the development of organs and systems is now completed.
To prevent complications, which in particular circumstances can also become important, it is however essential to maintain the glycemic balance within the recommended limits, with a renewed gesture of love towards oneself and the little one.
Symptoms and Risk Factors
For further information: Gestational Diabetes Symptoms
The symptomatology of gestational diabetes is most often absent. Rarely, the pregnant woman may notice signs and symptoms typical of hyperglycaemia, such as increased thirst (polydipsia) and urination (polyuria), nausea and vomiting, urinary infections and blurred vision.
Low risk of gestational diabetes
- age <25 years
- normal weight before pregnancy
- normal birth weight
- ethnicity with low prevalence of gestational diabetes
- absence of diabetes in first degree relatives
- absence of previous hyperglycemia
- absence of previous obstetric problems
NOTE: Screening Glucose Tests are NOT required ONLY if all of the above criteria are met.
High risk of gestational diabetes
- positive family history of diabetes in first degree relatives
- previous history of GDM, impaired glucose tolerance, impaired fasting glucose or glucosuria
- macrosomia in previous pregnancies
- obesity
- marked glycosuria in ongoing pregnancy
NOTE: Perform blood glucose tests as soon as possible if one or more of the above conditions are present.
Medium risk of gestational diabetes
- patients who do not meet the high risk or low risk criteria
Additional risk factors
- Smoking and polycystic ovary syndrome
Screening
Precisely because of its tendency to proceed in an asymptomatic or paucisymptomatic manner, the identification of gestational diabetes cannot be separated from careful screening, even more important if it is seen as a precious opportunity to reduce the frequency of maternal and fetal morbidity, and various complications .
The term screening designates a clinical procedure that has no diagnostic purpose, but simply to identify a subgroup at risk for a given pathology. For the definitive diagnosis, individuals tested "positive" to a screening test must therefore undergo a further assessment, which - if positive - will allow an early treatment capable of producing the best possible benefit.
Depending on the bibliography and the guidelines consulted, this screening:
- it must "be universal, ie conducted on all pregnancies between the 24th-28th week of gestation, possibly anticipating it to the 14th-18th in the presence of serious risk factors (strategy followed by many centers);
or:
- it is not necessary in low-risk women;
- it should be performed between the 24th and 28th week of pregnancy in women at medium risk;
- it should be performed as early as possible, ie between the 14th and 16th week, in high-risk women, who also - in case of negativity - must undergo the test again at 24-28 weeks. The risk identification criteria are shown in the table opposite and for obvious reasons they should be identified before the onset of pregnancy.
Diagnosis
There is currently no unambiguous international consensus on the methods of screening and diagnosing gestational diabetes; for the same reason there is no uniformity in the epidemiological data. The incidence of gestational diabetes - which has increased significantly in recent decades, probably due to sedentary lifestyle, changed eating habits and the "increase in the average age of pregnant women - can be estimated in 10-20% of the population over the age of 35 years old and, as far as the Italian one is concerned, about 6% (average figure which takes into account all age groups).
The most popular screening method is called GCT, which stands for Glucose Challenge Test. Basically, it is a glucose load test with 50 g of glucose and blood glucose determination 60 minutes after ingestion of the glucose solution.
If after one "hour the glycaemia is greater than or equal to 140 mg / dl, but less than 180 mg / dl (7.8-10.2 mmol / L), the test is positive, even if we cannot yet speak of gestational diabetes. to obtain diagnostic confirmation, oral loading must be carried out with 100 grams of glucose (OGTT), this time fasting for 8-12 hours. It is not necessary to resort to this test if the glycaemia exceeds 198 mg / dl, an element already per self sufficient to diagnose diabetes. During the OGTT at 100 grams, blood sugar is measured at regular intervals, fasting and 60, 120 and 180 minutes after ingestion of the first sip of glucose solution: if two or more glycemic values are higher than the reference values, gestational diabetes is diagnosed; if only one value is higher, glucose intolerance is diagnosed during pregnancy.
OGTT at 100 g for the research of
gestational diabetes,
interpretation of results,
limits of normality
Less than 95 mg / dL or 5.2 mmol / L
Less than 180 mg / dL or 10.0 mmol / L
Less than 155 mg / dL or 8.6 mmol / L
Less than 140 mg / dL or 7.7 mmol / L
Learn more about running the GCT AND OGTT tests
If the suspicion of manifest hyperglycaemia is high (eg presence of polyuria and polydipsia), measurement of the basal blood glucose may be sufficient to confirm the diagnosis of diabetes; in this case a baseline blood glucose value >126 mg / dl or an occasional value >200 mg / dl are to be considered diagnostic for diabetes mellitus, as long as confirmed by a second control.
Longitudinal studies are underway to evaluate whether the standard glucose load test (approved for non-pregnant subjects) in one phase with 75 g of glucose and glycemic control 2 hours after loading, can be applied instead of loading. carbohydrate of 100 g described above.The forthcoming data should therefore dampen the "endless" controversy on the diagnosis of gestational diabetes, proposing a homogeneous reference model.
Other articles on "Gestational Diabetes"
- Gestational diabetes: risks, prevention, treatment
- Gestational Diabetes - Medicines for the Treatment of Gestational Diabetes
- Diet and Gestational Diabetes



.jpg)