The disease initially manifests itself with profuse tearing, pain, foreign body sensation, hypersensitivity to light, conjunctival redness and blurred vision. Relapses of herpetic keratitis can cause neovascularization of the cornea (usually clear and devoid of vessels), permanent scarring and decreased vision.
The diagnosis is based on the presence of the characteristic dendritic corneal ulcer which stains with fluorescein upon examination with the slit lamp. With adequate treatment, the symptoms of herpetic keratitis usually resolve within a few weeks. that topical and, occasionally, systemic antiviral drugs do not clear the virus, but help bring it back into a latent state.
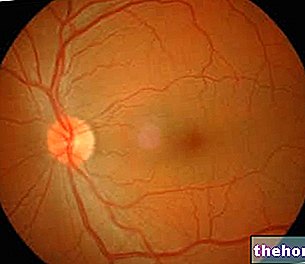
and the pupil. Normally transparent, this structure represents the first "lens" that light encounters on its way to the brain. The cornea is, in fact, an essential element of the ocular dioptric system: it allows the passage of light rays towards the internal structures of the eye and, together with the lens, helps to focus the images on the retina.
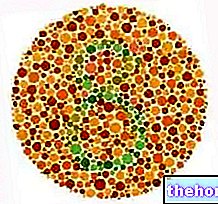
The cornea is made up of superimposed layers, the outermost of which is the stratified paving epithelium, while the subsequent ones are formed by a dense interweaving of collagen fibrils arranged in lamellae, with a glycoprotein matrix that unites them and makes them transparent.
Herpetic keratitis represents one of the most serious ophthalmological problems as it can determine the loss of corneal transparency with reduced vision. The inflammation underlying the inflammatory process is related to herpes simplex virus (HSV) infection.
and their edges; sometimes, however, it can also involve the conjunctiva, cornea and other ocular structures. Herpes simplex penetrates the organism through the skin and mucous membranes, where it infects the epithelial cells and causes their death, resulting in vesicles filled with serum-blood secretion and other typical lesions of the disease.