Synovitis can also affect other structures adjacent to the synovium, belonging to the joint (arthrosynovitis) or to tendon formations (tenosynovitis). The causes that determine its onset can be different (infections, trauma ...); it can also occur in association with arthritis, gout and lupus.
Synovitis can be acute (due to trauma or infectious factors) or chronic (due to diseases such as tumor proliferation or rheumatoid arthritis).
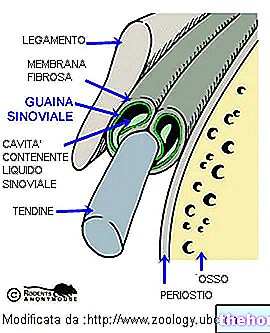
In short: anatomical structures and functions of the joint

The synovial fluid fills the joint cavity: it is produced by the vascularized synovial membrane which secretes the fluid by plasma filtration (in synovitis the joint swells due to the collection of synovial fluid).
The synovial fluid is also contained within the synovial bags; function of these anatomical elements is to protect the structures between which they are interposed (bones, tendons and muscles): they reduce the friction between the bones, allow free movements, determine a better distribution of the load and stresses to which the joints are subjected.
Synovial fluid is also contained inside the synovial sheaths, anatomical structures that line the tendons to reduce friction from rubbing along their course
Image source: http://www.mdguidelines.com/synovitis
Symptoms common to all forms of synovitis include swelling (swelling) associated with local pain, serous joint effusion and limitation or even inability to move the affected joint. The area affected by synovitis appears swollen, warm (due to increased blood flow , caused by inflammation) and painful (for example, in the case of the knee especially when trying to extend the leg). In the event of an infection, the skin on the knee may also be tight and red. In case of chronic progression of the disease, the synovial membrane can thicken and erode the underlying bone, causing further pain and degenerative changes, sometimes the appearance of inflammatory nodules.
general (example: rheumatic fever), dysmetabolic affections, lupus, arthrosis, rheumatoid arthritis, synoviomas (tumors of the synovial membrane).The forms of acute synovitis are due to trauma or secondary to infectious diseases (example: septicopemia, cerebrospinal meningitis, scarlet fever, abdominal typhus, etc.) and can be exudative: the inflammatory fluid infiltrates the thickness of the membrane and collects in the joint cavity mixing with the synovial fluid.
The forms of chronic synovitis can be bacterial in nature (syphilis, tuberculosis) or due to particular conditions; they can cause degeneration of the joint, suffering of the articular cartilages and arthrosis.
The consequence of synovitis is inflammation of the tendon relative to the affected joint, which tends to become chronic and degenerate.
detailed description of the patient and continues with the medical examination, which allows to identify the general clinical characteristics of the inflammation (heat, redness and swelling). In some cases, to reach a definitive and more precise diagnosis, the specialist can use diagnostics for images (radiographs, magnetic resonance or computerized axial tomography) and arthroscopy. The analysis of the aspirated synovial fluid allows to confirm or exclude several common diseases, such as traumatic or rheumatoid arthritis, osteoarthritis, gout and arthritis. . The analysis subjects the viscous and transparent fluid secreted by the synovial membrane to clinical investigation, to define a diagnosis quickly, at low cost and unequivocally; it also provides indications on the inflammatory or non-inflammatory nature of the joint effusion through a simple count leukocyte, and allows us to formulate hypotheses on any septic forms, which, in any case, require microbiological confirmation.
No special preparations are required prior to sampling. The skin over the joint is disinfected and a local anesthetic is usually injected. Using a fine needle, the doctor takes a sample of fluid for analysis; the latter includes the culture of the fluid when the infection is a possible diagnosis (the infectious factors / pathogenic bacteria responsible for the primary disease are found) and the examination of the microcrystals to diagnose gout (relevant in the rheumatological field: the finding of the monosodium urate and calcium pyrophosphate allow, in fact, the instant diagnosis of gout and pseudogout).
The analysis of the synovial fluid is often able to provide useful elements for diagnostic and therapeutic purposes: the examination can be useful to evaluate the evolution of the joint pathology, or to verify the effects of the therapy.
The chemical-physical characteristics of the synovial fluid are represented by quantity, viscosity, appearance and color (clarity, presence of blood and / or pus):
Macroscopic characters found in the synovial fluid
Color
Appearance
Viscosity
Synovial fluid
Light yellow
Transparent
Preserved
Non inflammatory
Dark yellow
Cloudy
Reduced
Inflammatory
Greenish-yellow
Purulent or milky
Variable
Septic
The microscopic investigations on the synovial fluid include: the leukocyte count, the cytological formula of the cells possibly present in the liquid, the microbiological examination and the observation of the fresh preparation (a liquid drop is deposited on a slide and observed with an optical microscope to search the presence of cells, crystals, etc.).
To confirm the diagnosis of synovitis it is possible to proceed with histological analysis by means of needle biopsy in order to study the characteristics of the synovial membrane under the microscope.
Synovitis: Conservative and Surgical Care and Therapies