
A pulmonary nodule can be benign or malignant in nature; in the first case (benign nature), it presents in the list of possible causes conditions such as tuberculosis, histoplasmosis, aspergillosis, sarcoidosis, rheumatoid arthritis and some particular types of benign tumor; in the second case (malignant nature), however, it is the result of cancerous processes (it is, that is, a malignant tumor).
Pulmonary nodules have a tendency to be asymptomatic, except when they are large in size.
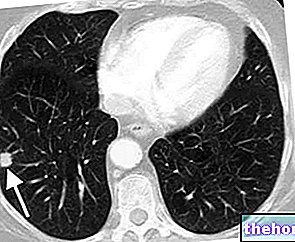
To identify a pulmonary nodule, it is essential to resort to diagnostic imaging, particularly chest x-ray or chest CT.
The therapeutic approach to a pulmonary nodule varies according to the nature of the formation: if no specific treatment is needed for benign pulmonary nodules, surgical removal is essential for malignant pulmonary nodules.
Benign Pulmonary Nodule and Malignant Pulmonary Nodule: the main differences
To distinguish benign pulmonary nodules from malignant pulmonary nodules are:
- The dimensions. Benign lung nodules rarely exceed 3 centimeters in diameter; the malignant pulmonary nodules, on the other hand, almost always have a diameter greater than 3 centimeters;
- The speed of growth. Benign lung nodules grow very slowly; malignant pulmonary nodules, on the other hand, are capable of doubling their size in less than 30 days;
- The frequency of appearance. Benign pulmonary nodules are definitely (and fortunately) more common than malignant pulmonary nodules.
- The consequences on the functionality of the lungs. Benign pulmonary nodules rarely alter lung function, while malignant pulmonary nodules drastically affect it.
So, in summary, compared to malignant pulmonary nodules, benign pulmonary nodules are smaller, grow very slowly, characterize most pulmonary nodule diagnoses, and only rarely compromise lung function.
Clarification on the denomination of large pulmonary nodules
Pulmonary nodules larger than 3 centimeters in diameter are more properly called lung masses.
supported by Mycobacterium tuberculosis (tuberculosis) or Mycobacterium avium intracellular and fungal infections caused by Aspergillus (aspergillosis), Histoplasma capsulatum (histoplasmosis), Coccidioides (coccidiomycosis), Cryptococcus neoformans (cryptococcosis).Pulmonary nodules associated with the above infections are examples of granuloma; a granuloma is a cell cluster, which appears as a result of an inflammatory process aimed at isolating substances considered foreign to the organism.
Causes of Malignant Pulmonary Nodule
Malignant pulmonary nodules are always the result of malignant tumor processes; in fact, they can represent the onset of cancerous forms, such as lung adenocarcinoma, lung lymphoma, lung carcinoid or lung sarcoma, or the result of metastases that have reached the lung from a malignant tumor that has arisen elsewhere.
What is a tumor? When is it benign and when is it malignant?
A tumor is a mass of very active cells, capable of dividing and growing uncontrollably.
- A tumor is called benign, when the growth of the cell mass is not infiltrative (that is, it does not invade the surrounding tissues) or even metastasizing.
- A tumor, on the other hand, is called malignant (or cancer or malignant neoplasm), when the abnormal mass of cells has the ability to grow very quickly and spread to surrounding tissues and the rest of the body.
WHO IS MOST AT RISK OF DEVELOPING A MALIGNANT LUNG NODULE?
Statistics in hand, the people in which it is more frequent to find a malignant pulmonary nodule are smokers (NB: cigarette smoking is the main risk factor for lung cancer), the elderly and those who, for various reasons, are been exposed for long periods to asbestos or other carcinogenic substances.
Epidemiology
- In most cases, the appearance of a pulmonary nodule has a "benign" origin;
- The likelihood of a pulmonary nodule to be malignant increases with the size of the formation; in fact, according to the most reliable estimates, if only 10% of pulmonary nodules with a diameter of less than 2 centimeters are malignant, 40-50% of pulmonary nodules with a diameter greater than 3 centimeters are malignant;
- According to some studies, malignant pulmonary nodules are, in almost 50% of cases, examples of lung adenocarcinoma;

- The risk of tracing a malignant pulmonary nodule in a person increases in parallel with age; in fact, this risk is equal to 3%, for subjects under the age of 39 years; it reaches 15%, for individuals aged between 40 and 49 years; it exceeds 50%, for those over 60 years old;
- The finding of a malignant pulmonary nodule is more common in smokers and the elderly.
The symptoms of conditions typically related to the appearance of an isolated pulmonary nodule are of enormous help in suspecting the presence of the latter and looking for it with specific diagnostic tests.
When is a Symptomatic Pulmonary Nodule most likely to be seen?
The likelihood of encountering a symptomatic pulmonary nodule is greater, when the formation has a malignant nature. This is related to the general tendency of malignant pulmonary nodules to be larger than benign pulmonary nodules.
Possible Manifestations of a Symptomatic Pulmonary Nodule
The symptoms that can arise from a pulmonary nodule are few and consist, essentially, in: cough, cough with consistent production of sputum, hemoptysis (ie cough with blood emission) and haemophtoe (ie presence of blood in the sputum).
Complications
The presence of a pulmonary nodule can give rise to complications, when the nature of the formation is malignant.
Specifically, in these circumstances, the possible complications are a profound impairment of the respiratory faculties and general health, and the spread of metastases to other parts of the body (eg brain or bones).
The complications associated with malignant pulmonary nodules are the result of an "evolution of these formations, which has increased their size and caused part of its constituent cells to be dispersed (metastases).
chest-related, such as chest x-ray (or chest x-ray) or chest CT (or chest CT).These instrumental tests, in fact, are able to photograph the internal thoracic organs (therefore, bones, heart, lungs, large vessels, etc.) and reproduce them, through one or more detailed images, on a special film (the so-called radiological plate).
Chest x-ray and chest CT scan compared
- Chest x-ray is less effective than chest CT at identifying a pulmonary nodule; however, it exposes the patient to significantly less harmful ionizing radiation.
- Chest x-ray is able to identify pulmonary nodules at least 1 centimeter in size; chest CT scan, on the other hand, can show pulmonary nodules as large as 1-2 millimeters;
- Of a pulmonary nodule, the chest x-ray provides a poorly detailed image, from which only characteristics such as shape, position and size are understood; the CT scan, on the other hand, ensures a rich reproduction of information, so much so that the doctor is sometimes able to establish the internal density of the training.
Did you know that ...
Only one in 500 chest x-ray reveals a pulmonary nodule in people who carry it.
What is the next step in identifying a Pulmonary Nodule?
It is the practice that, immediately after the detection of a pulmonary nodule, all those diagnostic investigations that are useful to establish the cause of the abnormal formation and its nature begin.
The list of diagnostic investigations in question certainly includes the medical history, physical examination, blood tests and a second radiological examination some time after the first, and, in particular situations, it could also include PET and a biopsy. pulmonary.
HISTORY AND OBJECTIVE EXAMINATION
In the context of a pulmonary nodule, the medical history and physical examination serve to clarify two aspects:
- If the patient suffers or has suffered in the past from symptoms that may in some way be linked to one of the possible causes of a pulmonary nodule (eg: a recent history of fever, night sweats, fatigue, etc. it could be the consequence of a "sustained infection. from Mycobacterium tuberculosis).
- If the patient falls into any risk category for malignant pulmonary nodules (ex: you are a smoker, are elderly, etc.).
WHAT IS A SECOND RADIOLOGICAL EXAMINATION FOR?
A second chest X-ray performed some time after the first (e.g. one month) is used to see if the pulmonary nodule has enlarged or changed its appearance.
Did you know that ...
Malignant pulmonary nodules are not only larger than benign pulmonary nodules, they are also more irregular in shape.
The analysis of the shape of a pulmonary nodule is part of the investigations useful to understand the nature of the formation.
LUNG BIOPSY
Lung biopsy consists of taking and analyzing in the laboratory a sample of suspicious lung tissue.
Pulmonary biopsy performed on a pulmonary nodule allows to accurately establish the nature of the formation; in this sense, it is the most accredited test.
The use of lung biopsy to study the nature of the pulmonary nodules occurs only when the previous examinations were not very exhaustive and doubts still remain.





















-nelle-carni-di-maiale.jpg)




