Generality
Optic neuritis is "inflammation of the optic nerve. This condition, which can involve partial or complete loss of vision, is usually caused by infections, autoimmune diseases, or damage to the optic nerve (from compression, tumor or ischemia). The onset" of optic neuritis is typically characterized by a triad of clinical signs: decreased visual acuity, ocular pain and altered color perception.

Causes
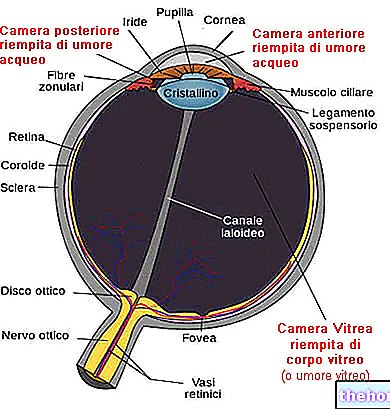
The optic nerve transmits visual information, coming from the retinal ganglion cells (located at the bottom of the eyeball), to the visual cortex located in the occipital lobe (area of the brain responsible for processing electrical stimuli in visual images). When the optic nerve is inflamed, its function is impaired; in particular, optic neuritis causes reduced vision due to swelling and degeneration of the myelin sheath that covers and protects the optic nerve. Under normal conditions, this sheath insulates the optic fibers, preventing to the electrical impulse that runs through them to disperse. Myelin damage then alters the normal transmission of electrical signals from the retina to the brain.
Optic neuritis can arise when the immune system mistakenly attacks the myelin sheath, resulting in partial or total destruction of the myelin sheath. Direct axonal injury can also contribute to optic nerve damage and impair its ability to conduct electrical impulses. However, the most common cause of optic neuritis remains multiple sclerosis (MS), a disease in which the immune system attacks the myelin sheath that covers the nerve fibers in the brain and spinal cord, resulting in inflammation and damage to the nerve cells involved. Optic neuritis is the most common visual disorder associated with multiple sclerosis and is often the first symptom to appear in a person with this demyelinating disease. Optic neuritis is a strong predictor for the development of MS; in fact, almost half of patients with optic neuritis have lesions of the white matter of the brain, detectable by magnetic resonance and consistent with the clinical picture of multiple sclerosis.
Other autoimmune diseases that can cause inflammation of the optic nerve are:
- Optic neuromyelitis (or Devic's syndrome, affects the optic nerves and spinal cord, but does not cause brain damage like multiple sclerosis);
- Systemic lupus erythematosus;
- Behçet's disease;
- Sarcoidosis.
Infections that can cause inflammation of the optic nerve are:
- Lyme disease;
- Syphilis;
- Meningitis;
- Viral encephalitis;
- Chickenpox;
- Rubella;
- Measles;
- Mumps;
- Shingles;
- Tuberculosis.
Other causes of optic neuritis can include:
- Nutritional deficiencies (example: vitamin B12);
- Toxicity from drugs or toxins (such as amiodarone, isoniazid etc.);
- Head radiotherapy;
- Drug-induced vasculitis (chloramphenicol, ethambutol, etc.);
- Temporal arteritis;
- Diabetes.
Finally, any process that causes inflammation, ischemia or compression of the optic nerve, including primary and metastatic tumors, can interfere with the ability to properly conduct electrical impulses through the optic pathway.
The disease mainly affects adults, aged between 18 and 45 years.
Symptoms
For further information: Optic Neuritis Symptoms
The main symptoms of optic neuritis can include:
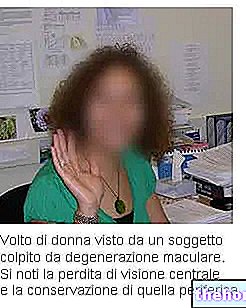
- Gradual or sudden loss of vision (partial or total), usually in only one eye
- Pain, which worsens with movement of the affected eye;
- Discromatopsia: reduction in the perception of colors, which appear faded and lacking in vibrancy (especially red);
- Severe blurred or "clouded" vision, which can progress to temporary blindness;
- Reduced sensitivity to contrast;
- Visual phenomena, such as perception of bright flashes in the absence of light (phosphenes), flashing lights and spots in the visual field (floaters, also called "flying flies" or "Floating bodies");
- Slow response to changes in light.
Simultaneous loss of vision in both eyes is rare but can occur during recurrent episodes of optic neuritis. In some people, symptoms may worsen temporarily with rising body temperature, exercise, hot and humid weather, sun exposure, or fever (Uhthoff's phenomenon). This effect is caused by inhibition of nerve conduction in the axons. partially demyelinated. Uhthoff's phenomenon resolves as soon as the body temperature returns to normal.
After onset, symptoms may worsen over the course of a few days or weeks, and then gradually resolve. If these do not improve after 8 weeks, a condition other than optic neuritis may be present.
Complications
Possible complications of this condition can include:
- Decreased visual acuity: Most people regain normal vision within a few months. Sometimes, vision loss may persist even after optic neuritis improves.
- Optic nerve damage: Most patients have permanent damage to the optic nerve after an episode of optic neuritis, but may not experience symptoms resulting from this condition.
- Side Effects of Treatment: Long-term use of corticosteroid medications can cause thinning of the bones (osteoporosis) and make the body more susceptible to infections. Other possible side effects of therapy include weight gain, mood swings, disturbances. stomach and insomnia.
Diagnosis
Optic neuritis is suspected in patients with a typical triad of clinical signs: decreased vision, eye pain, and impaired color perception. Eye and neurological examinations can provide a correct diagnosis: characteristic findings may include impaired peripheral vision, impaired pupillary reflex, decreased perception of brightness in the affected eye and swelling of the optic disc.
To establish the diagnosis of optic neuritis, an ophthalmologist can perform the following investigations:
- Eye exam: The ophthalmologist will check visual acuity and color perception. Vision is impaired proportionally to the extent of the optic neuritis. In many cases, only one eye is affected and patients may not be aware of the altered color perception, at least until they are asked to close or cover the eye. "healthy eye.
- Ophthalmoscopy: This test allows you to examine the structures in the back of the eye (ocular fundus), using an ophthalmoscope. The ophthalmologist will pay particular attention to the optic disc, the area of insertion of the optic nerve on the retina. it is not always found, in about 33% of people with optic neuritis, the optic disc appears swollen (anterior papillitis) and there may be dilation of the blood vessels around the nerve. However, the optic nerve often does not have any visible abnormal appearance to ophthalmoscopic examination, since the inflammation is entirely retrobulbar (retrobulbar optic neuritis).
- Pupillary reflex to light: the examination allows to measure the integrity of the sensory and motor functions of the eye. The ophthalmologist moves a lamp in front of the eyes to evaluate the reaction of the pupils to the light source. The optic nerve constitutes the afferent pathway of the pupillary reflex, that is, it perceives incoming light. If this is affected by inflammation, a defect in the reaction of the pupils may be found. The compromise of the optic nerve causes, in fact, a lower pupillary narrowing in response to the light stimulus, since the signal collected by the damaged optic nerve is unable to reach the brain.
- Visual evoked potential: the doctor places small surface electrodes on the patient's head, to evaluate the electrical reaction of the brain to certain visual stimuli (it is recorded in a similar way to the electroencephalogram). During this test, the subject sits in front of a a screen showing a moving checkerboard pattern. Visual evoked potential highlights reduced electrical conduction of the optic nerve, which may represent damage. Optic neuritis can occur even without any symptoms. In other words, a "inflammation of the nerve tracts without the patient noticing changes in vision. For this reason the visual evoked potential can be useful in making the correct diagnosis.
- Optical Coherence Tomography (OCT): This is another painless and non-invasive test that can assess the health of the optic nerve. Optical coherence tomography can detect evidence of optic nerve demyelination and allows doctors to know if damage has occurred due to previous inflammatory processes.
It is important to remember that optic neuritis can be an initial symptom of certain pathological conditions. A full medical exam can help rule out any related diseases.
This can include:
- Blood tests: blood chemistry tests allow you to search for the presence of inflammatory parameters, such as ESR or C reactive protein. A high erythrocyte sedimentation rate (ESR) can help determine if optic neuritis is caused by "inflammation of the cranial arteries (temporal arteritis); in addition, blood tests can detect the presence of anti-myelin antibodies (to investigate diseases autoimmune) and signs of any viral and bacterial infections.
- MRI: A patient who has a first episode of optic neuritis usually undergoes an MRI to look for any lesions affecting the central nervous system. This imaging test allows you to perform a detailed scan of the structures involved in optic neuritis. During the investigation, a contrast agent may be injected to evaluate any changes in the optic nerve and brain. MRI, for example, can determine if the myelin has been damaged and can help diagnose multiple sclerosis. demonstrating the presence of characteristic anomalies.If the patient has atypical symptoms or if optic neuritis is associated with other neurological or ocular signs, the procedure can exclude or confirm the presence of tumors and other conditions that can mimic optic neuritis (ischemia or compression for various types of swellings) .
Treatment
In most cases, the prognosis is good: the disorder is only transient and vision improves spontaneously within a few weeks or months, unless an underlying condition is the cause of the optic neuritis. Patients may regain normal vision, but contrast sensitivity and color perception may remain slightly impaired.
If optic neuritis is determined by a specific infectious cause, appropriate therapy may be prescribed; eradication of the underlying infectious agent usually prevents further episodes.
When optic neuritis is related to multiple sclerosis, vision returns to normal within 2-12 weeks without treatment, but it can also progress to permanent low vision or blindness.
A therapeutic regimen with intravenous corticosteroid drugs (such as methylprednisolone) may be prescribed in order to accelerate recovery; however, high doses of corticosteroids should be used with caution to avoid possible side effects.
Intravenous therapy may be followed by a gradual reduction in the dose of corticosteroids, which can be taken orally for about 11-14 days (example: prednisone). In cases resulting from demyelinating diseases, such as multiple sclerosis, optic neuritis can be recurrent.
An immunomodulator (interferon, natalizumab, etc.) or immunosuppressive therapy (cyclophosphamide, azathioprine or methotrexate) may be prescribed to reduce the incidence of future attacks.
Continue: Drugs for the Treatment of Optic Neuritis "



















-nelle-carni-di-maiale.jpg)




