The testes are the male gonads. They therefore represent the primary reproductive organs of the male responsible for spermatogenesis, that is, the synthesis of spermatozoa (male gametes).

Small in the fetus and child, the testicles rapidly grow in volume on the threshold of puberty; in adults they reach a weight of about 10-20 grams each.
Equal in number (right and left testis) and symmetrical, or the testes have an ovoid shape. Hard-elastic consistency, in adulthood they have an average size equal to:
- 3.5-4 cm in length
- 2.5 cm wide
- 3 cm in anteroposterior diameter
The testicles are received in the scrotum, a cutaneous fibromuscular sac suspended below the pubic symphysis between the antero-medial faces of the thighs. Usually, the left testicle is lower than the right one, so the scrotum is also lower on the left side, and the ipsilateral spermatic cord is longer; this feature may have been selected in the course of evolution to prevent the testicles from bumping against each other.
During development, the testes form in the abdominal cavity, next to the kidneys. Subsequently, they move downward dragging ducts, vessels and nerves, which will form the spermatic cord. Shortly before birth or soon after, the testicles go to place themselves in the scrotal sacks. When this is not the case, we speak of cryptorchidism.

Inside the scrotal sac the two testicles are partially separated by a median septum of fibrous tissue (the scrotal septum). The external position of the scrotum, therefore the distance of the testicles from the pubic symphysis, is regulated by the dartos muscle and its ability to contract and relax as a function of temperature. In fact, if the temperature of the testicles rises, the synthesis of spermatozoa (spermatogenesis) is inhibited; consequently, in cold weather, the contraction of the scrotal muscles brings the testicles closer to the body, making the scrotal bursa appears more collected and wrinkled, while in a warm environment the scrotum appears elongated, smooth and flaccid.The cremaster muscle also helps to maintain testicular temperature, regulating its functioning.
The gubernaculum testis is a "fibrous appendix, a connective lamina that fixes the lower pole of the testicle to the scrotal bag. Inside the scrotum, the testicles hang from the lower end of the corresponding spermatic cord."
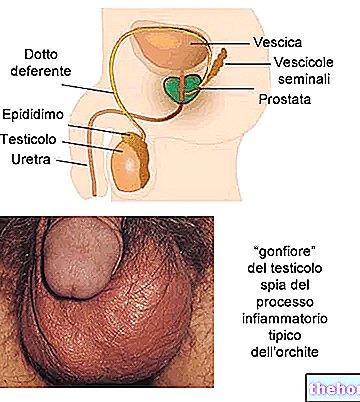
In addition to the testicles, the scrotum also houses the relative epididymis and the lower part of the spermatic cord:
- the epididymis is located against the posterior margin of the testicle; in its tail it collects the spermatozoa produced by the testicle and brought to maturity inside it; moreover, it participates in the control and changes in the composition of the seminal fluid, through secretion and absorption processes; finally, it contributes to the elimination of damaged spermatozoa. The epididymis constitutes the first stretch of the spermatic ducts and at its tail we find the beginning of the relative vas deferens
- during orgasm the spermatozoa are poured from the epididymis into the vas deferens, where they continue upwards thanks to the peristaltic action generated by the muscles of this connecting tube. They then flow into the ejaculatory ducts and from there into the prostatic urethra; during this process the spermatozoa join the secretion product of the accessory sex glands, such as the prostate and seminal vesicles.
- The spermatic cord is a cord that connects the testicle to the rest of the organism, gathering within it a set of structures (arteries, veins, lymphatic system, nerves, vas deferens, cremaster muscle, etc.) held together by loose connective tissue. 14 cm, for a diameter of 10 mm, the funiculus extends from the posterior margin of the testicle to the abdominal cavity of the inguinal canal, where it resolves into the various formations that constitute it.

The Testicle is made up of 2 main components:
- interstitial Leydig cells → secrete androgens (mainly testosterone)
- seminiferous tubules → constitute 90% of the weight of a mature testicle and are formed by:
- germ cells → synthesize spermatozoa (spermatogenesis)
- Sertoli cells → support the function of germ cells, both from a mechanical and functional point of view: they supply nutrients (lipids, glycogen and lactate) and substances with a regulatory activity for spermatogenesis
The testicle is wrapped in three cassocks, which - from the outside towards the inside - respectively take the name of
- vaginal tunic: double-walled serous membrane that wraps and stabilizes the testicle; consists of two sheets: parietal (periorchio) and visceral (epiorchio)
- cassock albuginea: located under the vaginal cassock, it is a layer of white-bluish fibrous connective tissue, which acts as a skeleton and scaffolding of the testicle
- vascular tunic: houses a plexus of blood vessels and delicate loose connective tissue
Fibrous septae originate from the albuginea tunic that run radially through the testicle, forming about 250-300 testicular lodges (or pyramidal lobules) separated by septa. These lobules have the shape of a pyramid with an enlarged base facing the albuginea tunic and the vertex located towards the mediastinum (or body of Highmoro), where they come together to form a fibrous body, which corresponds to the "hilum of the organ", which gives passage to efferent ducts, blood and lymphatic vessels, and nerves.
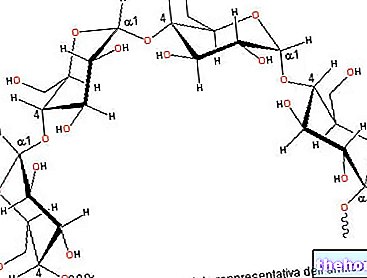
Each lobule contains from one to three to five thin contorted seminiferous tubules, which thanks to their tortuous course are able to occupy little space despite being 30 to 180 cm long.

At the terminal part, towards the posterior face of the testicle (mediastinum), the course of the contorted seminiferous tubules becomes rather straight and for this reason they are called straight tubules.

As anticipated, the epididymis is a maturation and storage chamber for spermatozoa until they are destroyed and absorbed by the surrounding tissue, or ejaculated.
The wall of the seminiferous tubules is made up of a multilayered epithelium, the germinative epithelium, in which we can distinguish support cells (or Sertoli) and germ cells. The spaces left empty by the seminiferous tubules are occupied by a loose connective which in addition to the various connective cells, it also contains the so-called interstitial cells of the Leydig, fibrocytes, blood and lymphatic vessels and a significant number of leukocytes (mainly macrophages and the lower grade T lymphocytes and mast cells).
- following stimulation by the LH, the interstitial cells of Leydig produce androgens (testosterone) starting from cholesterol carried by LDL or synthesized in the cell starting from acetate. Testosterone, in turn:
- It stimulates spermatogenesis and provides for the maturation of spermatozoa
- It monitors the activity of the spermatic ducts and related glands
- Determine secondary sexual characteristics
- It has an anabolic effect on protein metabolism
It determines sexual behavior by affecting the CNS
- the Sertoli cells
- They constitute the blood-testicular barrier: tight-junctions isolate the lumen of the seminiferous tubules from the interstitial fluid that surrounds them, preserving the development environment of the spermatozoa.
- Support for spermiogenesis: they provide nourishment and chemical stimuli to the gametes for their differentiation; mediate the effects of the FSH hormone
- ABP secretion: Androgen binding protein (essentially testosterone) inside the seminiferous tubules, stimulating spermatogenesis
- Secretion of the hormone inhibin, which inhibits the production of gonadotropins in the pituitary gland with a feed-back mechanism
- They perform phagocytic function
- They allow the movement of the germ cells towards the lumen
- the germ cells of the testes are involved in spermatogenesis: the primitive diploid seminal cells that rest on the basement membrane of the seminal tubule, just before puberty, differentiate into spermatogonia; these in turn - following hormonal stimuli - go against numerous differentiations that transform them into spermatocytes, spermatids and finally into spermatozoa through morphological modifications