Definition
The inflammatory process affecting the testicle, orchitis to be precise, can appear suddenly, with acute and excruciating pain, or it can arise gradually.In the introductory article, orchitis was described in a general way, examining its triggers, risk factors, and classification. In this brief discussion, the topic will be broadened and studied through the analysis of the typical symptoms of orchitis: in conclusion, possible therapies and hopes for recovery will be reported.
We have seen that the disease can have an acute or chronic course; based on this, it is clear that the symptoms differ according to the type of orchitis.
Typical Symptoms of Orchitis
For further information: Symptoms of orchitis

The affected subject also presents a slight alteration of the basal temperature (low-grade fever) which, often times, degenerates into a real fever, among other things almost never higher than 38 ° C.
The characteristic symptoms of chronic orchitis include: chills, stranguria (particularly slow and painful urine output), constant nausea, mild or severe testicular pain, abdominal tension, swelling of the inguinal lymph nodes and conspicuous redness The symptoms of orchitis can also affect the sexual act, causing a typical painful ejaculation.
It should be remembered that a patient suffering from orchitis does not generally present all the symptoms listed above: in fact, the disorders can be more or less severe depending on the subject and, again, the symptoms can arise at different times of the disease.
Complications
Like all genital diseases, orchitis should not be underestimated as, when neglected or untreated, it could worsen and cause irreversible damage. In particular, when the pain in the testicle is perceived as excruciating and unbearable, the doctor's opinion is absolutely necessary.
Orchitis can be directly or indirectly related to torsion of the testicle, therefore it would be imprudent not to consult a doctor. In such situations, the disease could in fact evolve in a negative direction causing irreversible lesions to the testicle, such as to make surgical removal of the diseased testicle.
It has been shown that chronic orchitis, and all chronic inflammation of the testicle, compromise spermatogenesis, generating alterations in the quantity, quality and morphology of spermatozoa; again, chronic forms - especially resulting from mumps - can cause testicular atrophy and inhibit the production of spermatozoa. It should be remembered that testicular atrophy often causes infertility, unfortunately, irreversible.
Another complication of orchitis is the formation of an abscess of the scrotum, which is filled with pus.
Hypotheses have been formulated, among other things not yet proven, concerning the relationship between orchitis and alteration of seminal parameters: in affected patients, the production of antibodies against the spermatozoa themselves, instigated by damage to the blood-epidimary barriers, is conceivable. and hemato-testicular. This correlation seems even more credible when, concomitantly with orchitis, the patient is also affected by epididymitis [taken from Clinical Andrology, by Wolf-Bernhard Schill, Frank H. Comhaire, Timothy B. Hargreave]
Diagnosis
The diagnosis of orchitis is a fundamental step, useful for identifying the problem and above all the cause that generated it. In this way, it is possible to opt for the most suitable therapy, according to the patient's symptoms. First of all, a careful clinical-anamnestic examination is advisable, useful for identifying any inguinal lymph nodes and the abnormal enlargement of one or both testicles. The ultrasound study is also very important for diagnostic purposes: in fact, genital ultrasound allows to identify a hypothetical enhancement of blood flow at the testicular level and to diagnose a possible torsion of the testicle.
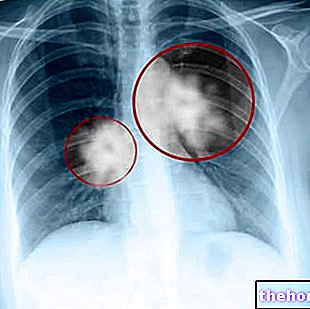
These investigations allow to highlight both any structural lesions of the didymus, and potential or hypothesized accumulations of transparent transudate around the testicle (hydrocele). In some cases of suspected orchitis, the doctor may request more in-depth clinical tests, such as blood culture.
Among the various diagnostic options, the doctor may recommend a urethral swab, in order to rule out or ascertain possible STDs. In some particularly problematic subjects from the diagnostic point of view, a testicular nuclear magnetic resonance is recommended.
"Orchitis should not be confused with epididymitis: differential diagnosis is required. Testicular torsion outlines the most relevant differential diagnosis of the acute form of orchitis, while chronic forms generally cause relatively milder disturbances."
Therapies
For further information: Drugs useful in the treatment of Orchitis
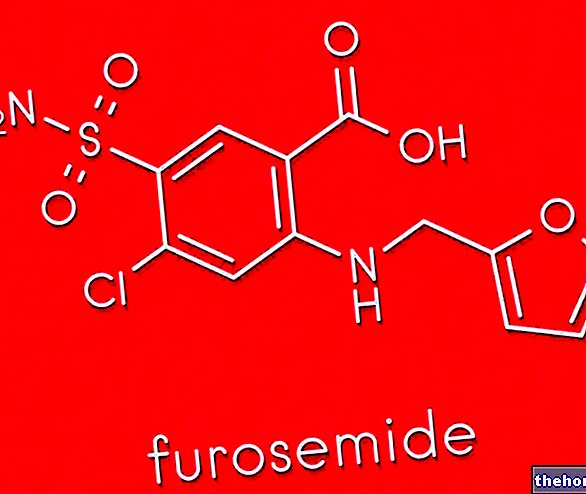
In general, the patient is given antibiotics and steroids. Specifically, antibiotics such as ciprofloxacin, azithromycin and ceftriaxone are particularly indicated against bacterial orchitis. When orchitis is caused by venereal diseases, the partner should also undergo antibiotic medical treatment.
Regarding viral orchitis, painkillers and anti-inflammatories are recommended (eg naproxen). The patient must also rest, preferably staying in bed; the topical application of ice at the scrotal level is useful for relieving pain and attenuating the swelling.
When the patient is also diagnosed with an accumulation of pus (pyocele) or in any case of purulent fluid in the scrotal sac, surgery is almost always necessary.
Prognosis
The prognosis is variable: it depends, in fact, on the severity of the disorder and on the way in which the patient responds to therapies. In some cases, orchitis can present itself in such a severe form as to generate irreversible sterility, while in other cases, infertility could be only a temporary phenomenon. Usually, mumps orchitis is the most dangerous form in terms of sterility: in fact, the hopes of regaining fertility again are not very high, especially when the start of therapy is postponed beyond the due.
Prevention
If mumps represents a serious risk factor for orchitis, it is clear that the first preventive practice is the vaccine against mumps. Another fundamental prophylactic measure consists in avoiding unprotected sexual intercourse, potentially dangerous for the transmission of venereal diseases.
More articles on "Orchitis: Symptoms, Complications and Therapies"
- Orchitis
- Orchitis - Drugs useful in the treatment of Orchitis
- Orchitis in Brief: Summary on Orchitis