In this video we continue to talk about hemorrhoids. Today, in particular, we will see together how it is possible to recognize, resolve and prevent their inflammation. Before proceeding, however, it is important to review some key points related to the disorder.
In the previous episode we saw that hemorrhoids are cushions of richly vascularized tissue, mainly with venous blood. They are placed inside the anal canal and play an important role in the mechanism of continence: by swelling they help to retain faeces, liquids and gases, while emptying they facilitate evacuation. When hemorrhoids undergo alterations and are irritated, they can increase in volume, bleed and protrude outside the anus, thus producing the characteristic symptoms of hemorrhoidal disease. In this regard we have seen that there is not a single cause, but several predisposing factors. To give just a few examples, the disorder can develop due to chronic constipation, excessive pressure to evacuate, a long stay squatting on the toilet, an unbalanced and low-fiber diet or pregnancy. Pathological conditions include liver cirrhosis, some pelvic neoplasms and prostatic hypertrophy. All these factors favor the congestion of the hemorrhoids; in practice, they fill with blood, dilating. The dilation favors on the one hand the lesion of the vessel walls and on the other, the collapse of the tissues of the anorectal wall which are forced to support a greater weight given by the accumulated blood. As a result, the hemorrhoidal veins bleed and tend to fall downwards, then to prolapse, dragging the mucous membrane that covers them with it.
Let's now see together how hemorrhoidal disease presents and develops. First, it should be noted that the symptoms are different depending on whether it is internal or external hemorrhoids. Internal hemorrhoids increase in volume inside the anus and typically show signs of themselves at the time of defecation. The most alarming symptom is bleeding. This bleeding can show up as bright red blood marks on toilet paper or as leaking after passing stool. Other times, blood drips down the toilet in copious amounts, in the form of bleeding. Pain, on the other hand, tends to be absent in the early stages and is more often linked to problems with anal fissures. Along with blood loss, prolapse is the most characteristic sign of pathological hemorrhoids. Over time, in fact, the internal hemorrhoidal cushions can protrude outside the anus; at first they do it only during defecation or other efforts and spontaneously return immediately afterwards; later, they require the help of their fingers to be able to re-enter. Finally, in the fourth and last stage, hemorrhoids permanently prolapse causing anal discomfort and pain, aggravated by the contracture of the anal sphincter. Other symptoms of the most serious stages are the loss of mucus associated with an annoying feeling of wetness, severe anal itching, burning and the urge to repeated bowel movements with loss of stool. Permanently prolapsed hemorrhoids can also be complicated by the formation of clots inside them. Thus, hemorrhoidal thrombosis occurs, a very painful acute inflammation. Other complications are the strangulation of external hemorrhoids, due to the contraction of the anal sphincter, the formation of anal or perianal abscesses, anemia and fecal incontinence. Before concluding this brief overview of the symptoms, it should be added that the disorder often tends to relapse; patients, in fact, experience alternating between acute crises and periods of relative relief of varying lengths. The frequency of symptoms is an important factor in planning the most appropriate therapeutic strategy for the case. When the intervals of well-being are increasingly rare despite all the attention to diet, hygiene and pharmacological aids, it is, for example, necessary to consider surgery.
The diagnosis of haemorrhoidal disease is obtained through a thorough proctological examination which, in addition to paying attention to the patient's clinical history, includes anal inspection, rectal examination and the execution of instrumental examinations. Visual inspection makes it possible to diagnose prolapsed hemorrhoids, fissures, fistulas, signs of infection or abscesses in progress and the presence of marische, that is the scarring of previous traumatic events. Digital exploration, on the other hand, is carried out by introducing the index finger well lubricated in the rectum; in this way it is possible to evaluate the tone of the anal sphincter, appreciate any abnormal masses or indurations and evaluate the health of the prostate in men and rectocele problems in women. In general, it is very important to arrive at a correct diagnosis that excludes other pathologies from similar symptoms, such as anal fissures, fistulas, abscesses or colorectal tumors. For this reason, diagnostic evaluation involves examining the anal canal through anoscopy, or the rectum and sigmoid through rectosigmoidoscopy. These tests make it possible to establish the extent of the prolapse of internal hemorrhoids; moreover, they allow to exclude other anorectal pathologies or neoplasms of the large intestine. For this reason, the complete study of the colon by colonoscopy or of its terminal tracts by means of rectosigmoidoscopy is indicated for patients over 50 years of age and with ongoing haemorrhoidal pathology; these tests, moreover, can also be indicated at an earlier age, around 40-45 years, in case of family predisposition for colorectal carcinomas.
As for the possible therapeutic interventions, it should be emphasized that the symptoms of hemorrhoids can be alleviated by acting above all on hygiene-food factors and lifestyle habits. These general measures form the basis of any treatment, whether pharmacological, surgical or phytotherapeutic; therefore diet and lifestyle corrections must always be implemented, regardless of any additional treatments. Among these treatments, in the mildest cases, there are drugs to be applied locally in the form of ointments, ointments and suppositories; such products do not "cure" hemorrhoids, but they can still relieve pain, discomfort and itching. Cortisones are mainly used in ointments, which have the effect of reducing inflammation, edema and itching, while local anesthetics, such as lidocaine, help relieve burning, pain and itching. These preparations, however, should be used only for short periods, as they can cause irritation of the anal area; moreover, it is good to rewind it, they must never be separated from the dietary and behavioral measures that we will see shortly. Some doctors can also prescribe phleboprotective drugs to be taken cyclically orally. examples are extracts of red vine, witch hazel, butcher's broom, sweet clover, horse chestnut, blueberry and hesperidin. The same extracts are also present in specific formulations for topical application, therefore in ointments to be applied at the anal level. Theoretically also useful are vitamin C and collagen supplements, which favor the trophism of the supporting connective tissues that keep the hemorrhoids anchored. inside the anal canal. Washes with warm water (around 40 ° C) are very effective in soothing local symptoms, while cold water should be avoided as it could lead to throttling of prolapsed hemorrhoids due to anal spasm.
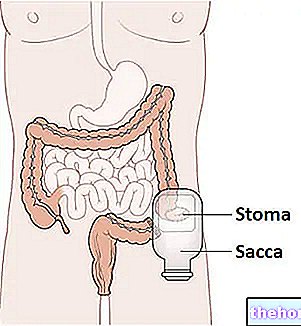
The concrete solution to relapses and progressive aggravation of the haemorrhoidal disease is surgical. Similar interventions should be considered in case of repeated failure of dietary-behavioral and pharmacological measures. In the initial stages of symptomatic disease it is possible to resort to outpatient treatments, which generally do not cause pain, but whose effectiveness is sometimes partial or transient. Among the most common interventions are elastic ligation and injection sclerotherapy. Elastic ligation consists in placing an elastic rubber lace at the base of the hemorrhoids, obtaining strangulation. The result is necrosis for the arrest of the blood supply and, after a few days, the spontaneous elimination of the bound tissue and of the elastic. The scar and the adhesions that form at the base of the treated area are also useful for preventing new prolapses. As an alternative to elastic ligation, sclerotherapy can be used. The method involves injections with sclerosing substances, in order to obtain a fibrous scar; the same result can be obtained by infrared coagulation, using the heat generated by a ray laser. The scarring reduces the flow of blood to the prolapsed area and creates adhesions that fix the hemorrhoidal mucosa to the underlying layers, preventing its prolapse. If, on the other hand, the hemorrhoids are present in a more severe and complicated form, it is necessary to resort to surgical techniques more complex in general or regional anesthesia. The traditional ones involve hemorrhoidectomy, ie the removal of hemorrhoids out of succeed outside. If the intervention is performed correctly, it is effective and decisive; however, the postoperative course is notoriously painful and there is a risk of incontinence. A more recent technique, called the Longo method, provides for the repositioning of the prolapsed hemorrhoids in their original position, without removing them; this allows to significantly limit post-operative pain and accelerate recovery from surgery. The same aim is pursued by the dearterilization technique (better known as the THD method). However, these innovative interventions also present some risks, so the choice of treatment the most suitable must be carried out on the basis of the characteristics of the patient and the experience of the surgeon.
We have repeatedly stressed how important prevention is, based above all on lifestyle changes and the adoption of some simple habits. A healthy and balanced diet, and regular physical activity, are in fact fundamental elements to counteract the exhaustion of the mucous membranes that contain the haemorrhoidal cushions. To maintain regular bowel function it is necessary to drink at least 1.5 - 2 liters of water during the day, chew slowly and focus on a diet rich in fiber, whole foods, fruits and vegetables. Instead, alcoholic beverages, the abuse of coffee and irritating foods, such as spices, sausages, fries and chocolate, should be avoided, which also accentuate the symptoms in the case of ongoing hemorrhoidal disease. In addition to stimulating bowel function and correcting constipation - which is an aggravating factor of hemorrhoids - a greater intake of fiber and fluids is also useful for keeping the stool soft. For the same purpose, on medical advice, the diet can be enriched with fiber supplements, such as guar gum, psyllium seeds and glucomannans. Furthermore, it is important to remember that in the act of evacuation you must always follow and support the stimulus, without trying too hard. For example, the feeling of fullness and incomplete emptying after defecation is common in patients with hemorrhoids; in these cases the patient may feel the need to further empty the intestine. It is however important to resist this stimulus to avoid excessive and unproductive efforts that could aggravate the disorder. You should not remain standing or sitting for too long, since in this way the stagnation of venous blood is favored. Regular physical activity is also very useful to massage the intestine, stimulating its functionality and thus preventing constipation.