which can be related to various conditions (eg anemia, recurrent infections, inflammation, coagulation disorders, etc.), therefore to ascertain a diagnostic suspicion and define a precise clinical picture;
Also called blood count, this test consists in the evaluation of the different parameters that refer to the main components of the blood:
- Number of all blood cells, i.e. the count of:
- Red blood cells (or erythrocytes): they contain hemoglobin which carries oxygen and carbon dioxide in the organism; they represent the most numerous blood cells. The erythrocytes have the shape of a biconcave disc (slightly flattened in the center) and have a characteristic red color (hence the name) due to their hemoglobin content, (iron-containing protein, necessary to transport oxygen in the blood). Red blood cells live an average of 120 days in the circulatory system and are subsequently removed in the spleen, so the bone marrow must continuously produce new ones in order to replace elements that have died, been destroyed or lost during a bleeding. "CBC includes: RBC count, hemoglobin (Hb), hematocrit (Hct) and red blood cell indices, which include mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscle hemoglobin concentration (MCHC), and, sometimes, the amplitude of the red cell distribution (RDW). The blood count may or may not include the reticulocyte (precursor to mature red blood cell) counts.
- White blood cells (or leukocytes): also known as leukocytes or WBC (White Blood Cells) - they are cellular elements of the blood responsible for the defense of the organism against infectious agents, foreign substances and other causes of damage. Leukocytes play an important role also in allergies and inflammations. The circulating white blood cells include very different cell populations, each of which with some specific functions and with a relatively stable percentage ratio from individual to individual: granulocytes (eosinophils, neutrophils and basophils) and cells mononuclear cells (lymphocytes and monocytes). The white blood cell count (evaluation of the total number of leukocytes present in the blood sample) is part of the blood count. These cells are present in the blood in a relatively constant quantity; their numbers may increase or decrease temporarily, depending on what happens in the body. The blood count may or may not include the differential count of white blood cells (leukocyte formula). This information identifies and counts the number of various types of leukocytes present and serves to understand if an "infection," allergy or a strong stress reaction is in progress in the body. In some conditions, such as leukemia, abnormal white blood cells (immature or mature) multiply rapidly, increasing their overall count.
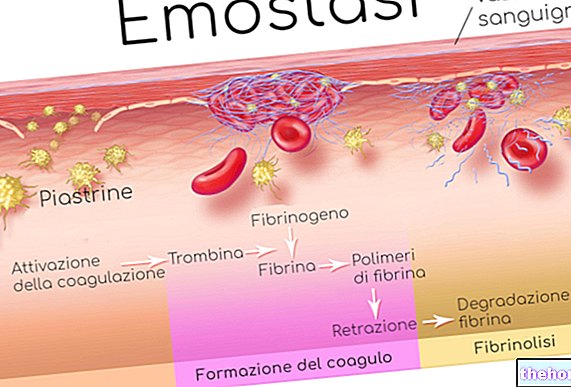
- Platelets (or thrombocytes): important for haemostasis and the coagulation process. Following trauma or small lesions in the blood vessel walls, the thrombocytes are transported to the area affected by the blood and attach themselves along the wound edges, progressively blocking the "hemorrhage. Any alterations to them can increase the risk of excessive bleeding or predispose to bruising. In the blood count, the count of these cell types is usually predicted; the assessment may or may not include the mean platelet volume (MPV) and / or the amplitude of platelet distribution (PDW).
- Leukocyte formula, i.e. the percentage amount of the different types of white blood cells:
- Neutrophils (50-80%): they are the most numerous white blood cells in the blood. Their primary function is to incorporate and digest microorganisms, abnormal cells and foreign particles (phagocytosis) by means of enzymes produced and secreted by them. Once they have migrated into the inflamed tissue and carried out their action, they die and - together with cellular debris and degraded material - form pus;
- Lymphocytes (20-40%): are observed both in the blood and in the lymphatic system. They differentiate from lymphoid stem cells in the bone marrow, making it possible to distinguish into different subpopulations with different functions. B lymphocytes secrete antibodies (Ab) - molecules important for the antigen-specific immune response, including the body's defense against infection - and mediate the humoral immune response (ie they are repositories of immunological memory). T lymphocytes induce a cell response -mediated (ie they are able to specifically recognize "self" antigens from "non-self" antigens), they produce cytokines that support the immune response of other cells and factors that destroy infected or neoplastic cells. In addition, T lymphocytes initiate and control the extent of the immune response and play an essential role in transplant rejection;
- Monocytes (2-8%): they are important in the defense of the organism from some types of bacteria; they secrete cytokines, phagocyte and digest foreign elements and damaged cells; they mature into macrophages in the tissues;
- Eosinophils (1-4%): they participate in inflammatory reactions and are mainly involved in the defense of the organism from parasitic infestations.Eosinophils also increase in allergic diseases (bronchial asthma, allergic rhinitis, urticaria, etc.) and may be responsible for some characteristic symptoms of these diseases;
- Basophils (1%): they are the least numerous white blood cells in the blood; they play a leading role in inflammation and allergic reactions during which they secrete chemical mediators, including histamine and heparin.

Shutterstock
- Hemoglobin (Hb): is a protein found inside red blood cells. Hemoglobin performs a fundamental function: to transport oxygen from the lungs to the tissues in all parts of the body. On its return journey in the blood venous, hemoglobin transports, instead, carbon dioxide to the lungs, from which this is expelled with the exhaled air. For this reason, it is important that its quantity is carefully evaluated: its deficiency leads to a state of anemia, as well as Weakness and various other disorders There are also various defects in the globin and heme genes. These can give rise to diseases such as thalassemia and porphyria.
- Hematocrit: Proportion of blood volume occupied by erythrocytes. This test is indicated as part of routine tests or when the doctor suspects that the patient has anemia (low hematocrit) or polycythemia (high hematocrit), as well as to assess hydration status.
- Corpuscular indices: it is the analysis of the physical characteristics (shape and size) of red blood cells and platelets, indicated by parameters typically included in blood tests as part of the blood count:
- MCV (mean corpuscular volume) is the measure of the average size of red blood cells;
- MCH (average cellular hemoglobin content) is the calculation of the average amount of oxygen-carrying erythrocyte Hb;
- MCHC (mean cellular hemoglobin concentration) is the average percentage of hemoglobin in red blood cells;
- RDW (width of red blood cell distribution) is an erythrocyte index that measures the variability in the size of red blood cells in peripheral blood.
- MPV (mean platelet volume) is a parameter that indicates the mean size of platelets.
ESR (Erythrocyte Sedimentation Rate)
The ESR is an inflammatory index which measures the speed with which the erythrocytes (red blood cells) of a blood sample - made uncoagulable - settle on the bottom of the tube that contains it. The parameter is expressed in millimeters of sediment produced in one hour and provides general information about the presence or absence of an inflammation and indirectly measures the degree of this state in the organism. It should be noted that the ESR is a non-specific (i.e. generic) index and must be interpreted in the context of other targeted clinical investigations. In other words, the finding of a high value should not cause concern, if other parameters are within the norm.
- For further information: ESR - Erythrocyte sedimentation rate
Fibrinogen
Fibrinogen is an essential factor for blood clotting; produced by the liver and released into the bloodstream when needed. When there is a wound and bleeding begins, a clot forms through a series of steps (haemostasis); in one of the last steps, the soluble fibrinogen is converted into insoluble fibrin filaments that intertwine with each other forming a network that stabilizes and adheres to the damaged site until healing.
The fibrinogen test is part of the investigation of a possible coagulation or hypercoagulability defect (thrombotic episodes). This investigation allows, in particular, to evaluate the concentration and functionality of fibrinogen. The test is also used to determine the risk of developing cardiovascular disease.
- For further information: Fibrinogen
Glycemia
Blood glucose is a test that is performed to understand if the concentration of glucose in the blood is within the normal range. Therefore, the test is useful for the screening and diagnosis of diabetes and prediabetes, as well as allowing the monitoring of patients who have high concentrations of glucose in the blood (hyperglycemia) and low concentrations (hypoglycemia).
Transaminases
Transaminases (also known as aminotransferases) are enzymes involved in amino acid metabolism and glucose synthesis. It is a rather large group of molecules, but the type of reaction in which they are involved is always the same: the transfer of the amino portion (the one containing nitrogen) from an amino acid to an acid molecule (called alpha-keto acid) to transform it into another amino acid.
Clinically, the two most important transaminases are aspartate transaminase (AST or GOT) and alanine transaminase (ALT or GPT).
The determination of transaminase levels in the blood are useful for evaluating correct liver function (ALT or GPT) but can also reflect the state of health of the heart and the musculoskeletal system (AST or GOT). The transaminase assay is used. both as a preventive measure and when the doctor suspects a malfunction or damage to these organs.
To know more:
- Transaminases
- Transaminases - AST and ALT
- Glutamic-oxaloacetic transaminase - AST or SGOT
- Alanine Amino Transferase, ALT
- Liver Values - Blood Tests
Alkaline phosphatase (ALP)
Alkaline phosphatase (or ALP, which stands for "alkaline phosphatase level") is an enzyme found in various tissues of the body. In particular, ALP is found abundantly in the bones and liver. Although in lower concentrations, alkaline phosphatase is also present in the intestinal cells, kidneys and placenta of pregnant women.
The alkaline phosphatase is measured to determine its circulating levels. This allows for screening or monitoring of bone or hepatobiliary diseases, as well as assessing whether ongoing therapies are effective.
- For further information: Alkaline Phosphatase (ALP)
Creatinine
Creatinine is the result of the breakdown of creatine phosphate (or phosphocreatine). This substance is mainly located in skeletal muscle and in the heart. For these tissues, creatinine is an immediately usable source of energy.
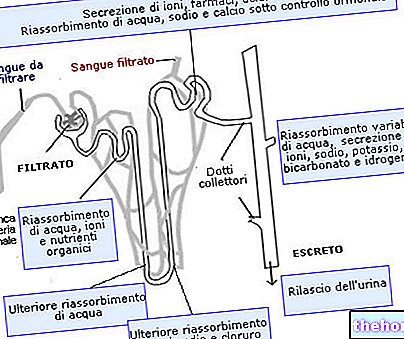
Once produced, creatinine is released into the blood. Subsequently, this is filtered by the renal glomeruli and is completely eliminated in the urine, without being reabsorbed at the tubular level.
The dosage of creatinine provides useful information about the efficiency of the functionality of the kidneys, being the latter the organs responsible for filtering the blood. This measurement takes place in two ways: through blood tests (creatinemia) and urine tests (24-hour creatininuria). If the presence of creatinine in the blood is too high, it means that the kidneys cannot pass it into the urine, so they are not doing their job well.
- For further information: Creatinine - Clearance and Creatininemia
Uric Acid (Uricemia)
Uricemia is the measure of the amount of uric acid present in the circulation.
Uric acid is a waste substance of cell metabolism, following the degradation of purines. Its concentration in the blood is the result of the balance between its production by the body and its elimination in the urine. uric acid is produced in excess or is not eliminated sufficiently, it can accumulate in the body and cause an increase in blood levels (hyperuricaemia).
The uric acid test is used to detect elevated levels of this compound to help doctors diagnose gout. This test is also used to monitor uric acid levels over time during certain therapies and as an aid in diagnosing the causes of recurrent kidney stone formation.
- For further information: Uricemia and Uric Acid
Total Bilirubin
Bilirubin is a substance that derives from the degradation of hemoglobin and, more specifically, from the conversion of the prosthetic group EME contained in it. Most of the bilirubin (85%) derives from the normal process of destruction of exhausted red blood cells. These cells in fact, they have a life of about 120 days: first they are degraded by the spleen and are incorporated in the biliverdin, then the residues are transported to the liver to be metabolized. The remaining part of the bilirubin comes, instead, from the bone marrow or liver. Under normal conditions, all the bilirubin that originates from hemoglobin is eliminated from the body with a mechanism that is usually found in equilibrium: what is produced is also processed to be degraded.
The bilirubin test measures its concentration in the blood to evaluate liver function or to diagnose anemia caused by damage or breakdown of red blood cells (haemolytic anemia).
- For further information: Bilirubin
Total Cholesterol and Triglycerides
The search for cholesterol in the blood contributes, with the search for triglycerides, to evaluate the lipid profile.
Cholesterol is a fat present in the blood, the largest share of which is produced by the body and only a minimal amount is introduced through the diet. The cholesterol associated with the so-called high density lipoproteins or HDL (High Density Lipoprotein) is considered "good" Instead of accumulating in the blood like the "bad" (LDL), the fraction of HDL cholesterol travels to the liver to be properly disposed of.
"Hypercholesterolemia is one of the main risk factors for the development of cardiovascular disease. More precisely, it is necessary to fear an increase in cholesterol transported by low-density lipoproteins or LDL, commonly called" bad cholesterol ". If it is in excess, this tends to accumulate on the walls of the blood vessels, forming thickenings and plaques, which obstruct the correct flow of blood and can lead to vascular ischemia. On the contrary, HDL cholesterol ("good cholesterol" carried by high density lipoproteins) lowers this risk: particles of HDL help cleanse the body of cholesterol, which they transport to the liver for elimination.
Albumin
Albumin is the most abundant protein in plasma. This is produced by the liver and has three main functions:
- Transport and eliminate waste substances that are expelled with the urine (such as bilirubin, fatty acids and hormones);
- Keep the oncotic pressure in balance, which regulates the water exchange between the capillaries and the interstitial fluid that surrounds the blood vessels;
- Build a reserve of amino acids (basic constituents of proteins) for the body.
The blood albumin concentration (albumin) is an indicator of the person's nutritional status and kidney or liver function. In addition, the blood albumin concentration reflects the person's nutritional status.
- For further information: Albumin
Ferritin
Ferritin is the main iron storage protein within cells. Its concentration in the blood reflects the extent of the mineral reserves in the body.
In clinical practice, the measurement of plasma ferritin (ferritinemia) is a useful parameter for evaluating the amount of iron available to the whole body.
- For further information: Ferritin

What Can Influence the Results of the Blood Test
Many medications interfere with the result, so it is always advisable to tell your doctor if you are undergoing any treatment. It is also recommended to abstain from alcohol consumption for at least 24 hours before the test.

















-nelle-carni-di-maiale.jpg)




