Congenital anomaly
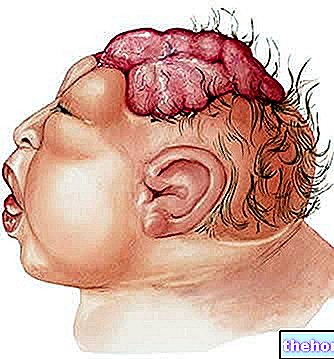
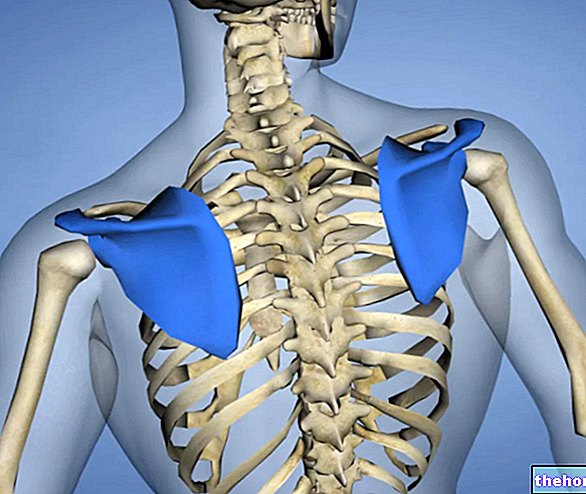
Among the malformations of the central nervous system, spina bifida plays a leading role: it is a serious congenital anomaly of the spine and spinal cord, which often severely compromises the patient's quality of life.
Although spina bifida is an incurable disease, it can be prevented: after a brief analysis of the diagnostic methods available, we will focus on preventive practices and current treatments aimed at relieving the symptoms induced by the disease.
Spina bifida is an extremely serious genetic defect: hence the need to sensitize the medical profession and the population on this complex health problem. Future mothers must be aware of the risk that their child could run: prevention is a tool concrete protection of health, both for the mother and for the unborn child.
Spina Bifida Diagnosis
Early diagnosis of spina bifida is essential to intervene promptly, limiting short and long-term damage as much as possible.
Thanks to the refinement of diagnostic strategies, it is possible to detect malformations of the spine (including spina bifida) even long before the birth of the child. The ultrasound and the numerous biochemical analyzes, in fact, allow to confirm a suspicion of spina bifida already in the 1st-3rd trimester of gestation.
What are the most accredited diagnostic techniques?
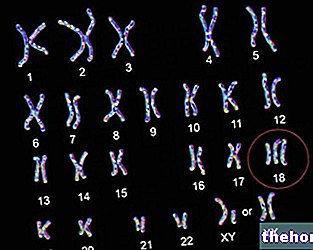
- Amniocentesis: minimally invasive technique consisting in taking a sample of amniotic fluid via the trans-abdominal route. Amniotic fluid contains amniocytes, specific cells from the fetus; after the isolation of the aforesaid cells, it is possible to carry out various molecular or cytogenetic analyzes on them.
- Ultrasound ultrasound: in addition to establishing the gestational age and the possible presence of several fetuses in the womb, this examination also highlights possible structural abnormalities of the unborn child (eg spina bifida).
- Blood analysis: any anomalies in the composition of the pregnant woman's blood can be an indicator of pathology, including spina bifida. An altered blood composition requires further investigation.
- AFP test (alpha-fetoprotein): alpha-fetoprotein is a glycoprotein with functions similar to those of albumin, which can be isolated from a serum sample. The substance is mainly synthesized during fetal life. If alphafetoprotein levels are high, the fetus is likely to have neural tube closure defects, a typical sign of spina bifida.
Prevention
Prevention is the best shield for defending the fetus from spina bifida, as well as the best care and protection for the unborn child. Thanks to the awareness campaign aimed at informing the population about this serious disease, the incidence of myelomeningocele has undergone a drastic decrease in recent decades.
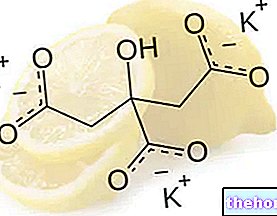
- Folic acid supplementation before conception and during pregnancy significantly reduces (by 50%) the risk of spina bifida in the unborn child.
Although many foods abound in folic acid, pregnant women need higher quantities than those recommended for the general population (400 mcg / day, compared to the classic 200 mcg / day); as a consequence, the intake of vitamin B9 with food alone may be insufficient to guarantee full protection from spina bifida. Hence the need to supplement the diet with specific folic acid supplements.
Natural sources of folic acid: oranges, whole grains, beans and legumes in general, liver, brewer's yeast, green leafy vegetables. Please note: folic acid is inactivated by prolonged cooking
Pregnant women who have already conceived a child with spina bifida must take an even higher dose of vitamin B9 (4-5 mg / day), in order to minimize the risk of giving birth to another child with the same disorder. .
If the parturient has a family history of spina bifida (parents, siblings, affected cousins), the fetus could still develop the spinal anomaly, regardless of the generous folic acid supplementation.
Among the preventive techniques we also remember the early diagnosis: the assessment of the disease during the first fetal stages will allow to perform, within the very first days of life, an emergency neurosurgical intervention to immediately correct the neural lesion.
Possible therapies
Let us remember once again that spina bifida is an incurable disease. The drugs and treatments currently available are indicated only to minimize the damage and complications of the disease.
Only the mild variant - spina bifida occulta - does not require any treatment, and runs almost always asymptomatically, without creating any kind of complications.
Let's see what are the most used medical treatments in case of spina bifida:
- The most severe forms of spina bifida (myelomeningocele and meningocele) require surgery to close the opening located at the level of the rachis. The "operation, extremely delicate, is essential to preserve the functions of the spinal cord and reduce the risk of" infection (e.g. meningitis).
- Other surgical strategies are aimed at draining the liquor (accumulated in the patient's brain) in the abdomen: the operation, indicated in the case of hydrocephalus, is performed by implanting a shunt (passage, hole) ventriculo-peritoneal.
- Prenatal surgery: Before the 26th week of gestation, surgeons can operate the unborn child directly in the womb. The surgery consists of opening the mother's uterus and subsequently repairing the baby's spinal cord.
Research is also being perfected in "in utero surgery, to minimize the damage caused by spina bifida to the unborn child.
- Further surgical interventions are aimed at fixing bladder and intestinal function: remember, in fact, that people with spina bifida often lose control of the anal and bladder sphincters.
Children with spina bifida will need to learn to use crutches and wheelchairs, as the disease also affects walking skills.
Although surgery is extremely effective in limiting the damage or correcting the disease as much as possible, an affected child will have to struggle with spina bifida for life.
Other articles on "Spina Bifida: Diagnosis, Prevention, Treatment"
- Spina Bifida: Signs or Symptoms
- Spina Bifida