Congenital CMV is much feared, since, being able to compromise the development of the fetus, it can cause deficits and malformations visible at birth; it should be noted, however, that the most severe forms of congenital CMV can even be fatal.
For the diagnosis of congenital CMV, a viral culture or PCR on a urine, saliva or body tissue sample is essential within the first week after the patient's birth.
For those born with congenital CMV, pharmacological therapy based on an antiviral such as Ganciclovir or Valganciclovir is envisaged.
The prognosis in case of congenital CMV varies from patient to patient, depending on the period of pregnancy in which the mother transmitted the cytomegalovirus infection to the fetus and on the severity of the infection itself.
Congenital CMV is preventable, as long as the mother avoids all those circumstances that expose her to Cytomegalovirus.
Congenital CMV is also known as "congenital cytomegalovirus infection" and "congenital cytomegalovirus".
.
It should be noted that, in very rare circumstances, the fetus can develop congenital CMV even when the mother has contracted the Cytomegalovirus infection within the 6 months prior to conception.
Cytomegalovirus: review of the main characteristics

Cytomegalovirus is a very common genus of virus, which belongs to the large viral family of herpes viruses, just like the most famous herpes simplex viruses, the varicella virus or the Epstein-Barr virus.
Responsible in people in good health of infections usually asymptomatic, with spontaneous resolution and without long-term consequences, the Cytomegalovirus could, for the reasons just mentioned, be of little interest from a medical-clinical point of view, were it not capable of :
- "Hiding" in the cells of the human being's bone marrow (example of viral latency), only to reactivate in a state of stress in which the infected person can find himself
And
- Cause serious consequences, when it infects people with an inefficient immune system (such as AIDS patients or organ transplant recipients) or pregnant women (NB: if in the first case the serious consequences directly concern the infected person, in the second case they are at the expense of the future unborn child).
Cytomegalovirus Infection in Pregnancy
We talk about Cytomegalovirus infection in pregnancy when a pregnant woman contracts Cytomegalovirus and develops the consequent infectious state.
Dangerous for the fetus, Cytomegalovirus infection in pregnancy can be primary or secondary: it is primary, when the infected mother has never contracted it up to that moment; it is secondary, however, when the infected mother has already contracted it in the past at least once.
Cytomegalovirus infection in pregnancy is particularly dangerous for the fetus when it is primary and occurs during the first three months of gestation; in fact, scientific evidence shows that primary infections in the second and third trimesters, and even more infections secondary encounter greater resistance in their harmful action towards the fetus.
It should be noted that, in terms of frequency, the transmission to the fetus of a "Cytomegalovirus infection in pregnancy is uncommon; according to statistics, in fact, the phenomenon would affect 30-40% of gestations, in the case of primary infection, and only 0.5-2% of gestations, in case of secondary infection.
Did you know that ...
In the "secondary type of cytomegalovirus infection in pregnancy, the antibodies of the mother developed by the mother at the time of the first encounter with the cytomegalovirus provide some protection to the fetus.
Transmission
The transmission of cytomegalovirus infection from mother to fetus occurs transplacental.
Transplacental transmission of cytomegalovirus is an example of vertical transmission of an infectious agent.
Epidemiology
In the world, one child for every 100-500 new borns is born with congenital CMV and one child for every 7000 patients with congenital CMV dies.
Congenital CMV is more frequent in the upper socio-economic classes of industrialized countries than in the poorest communities; this happens because in the poorest populations the number of fertile women immune to Cytomegalovirus is greater than in the richest populations and in which hygiene measures are better.
According to some estimates, in the industrialized countries of the world, 8% of mothers who are not immune to cytomegalovirus contract the cytomegalovirus infection in pregnancy and 30-40% of mothers with a cytomegalovirus infection in pregnancy transmit the infection to the fetus , triggering the so-called congenital CMV.
Congenital CMV is the most common congenital viral infection.
), both in the short and long term;It should be remembered that congenital CMV is more likely to have repercussions at the fetal level when it derives from a primary "cytomegalovirus infection in pregnancy, which occurred in the first 3 months of gestation.
Immediate Symptoms of Congenital CMV

The possible immediate consequences of congenital CMV include:
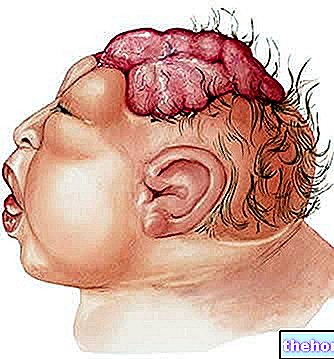
- Microcephaly;
- Low birth weight;
- Petechiae (they are small red spots on the skin, usually rounded, produced by microhematomas);
- Enlarged liver and enlarged spleen (hepatosplenomegaly) with jaundice;
- Retardation in growth;
- Abnormal deposits of calcium in the brain.
In severe cases, congenital CMV can even be fatal.
It is estimated that 80-90% of symptomatic congenital CMV cases develop complications at birth in the years to come.
Long-Term Symptoms of Congenital CMV
Possible long-term consequences (late symptoms) of congenital CMV include:
- Decrease or loss of hearing. Estimates say that these disorders affect one in seven children with congenital cytomegalovirus infection;
- Development and learning difficulties due to permanent neurological damage;
- Physical disabilities;
- Convulsions and epilepsy;
- Vision problems due to chorioretinitis.
It should be noted that a child with congenital CMV could develop problems related to the aforementioned infectious state up to the age of 12.
Furthermore, scientific studies have shown a certain correlation between congenital CMV and the development at a later time, compared to birth, of conditions such as autism and attention deficit hyperactivity disorder (ADHD).
According to some statistics, 5-10% of congenital CMV cases asymptomatic at birth develop disorders at a later age.
indicative of the condition and / or when the mother, during the pregnancy, contracted the Cytomegalovirus infection.How to detect Cytomegalovirus Infection in Pregnancy?

A simple blood test is sufficient to identify a "cytomegalovirus infection in pregnancy, whether it is current or previous."
On the blood sample taken from the patient, the analysis laboratory will evaluate the presence of specific antibodies directed against the viral agent in question: if these specific antibodies are present, it means that the patient has come into contact with the Cytomegalovirus; if instead they are absent, it means to say that the patient has never contracted the Cytomegalovirus infection.
In particular, the evaluation on the blood sample will concern the IgM and IgG class anti-Cytomegalovirus antibodies: the IgM antibody positivity indicates a recent "infection, while the IgG antibody one indicates a past contact with the virus without providing useful information. on the period of contagion.
For further information: Positive IgG Cytomegalovirus: what does it mean?Did you know that ...
During pregnancy, women who are not immune to cytomegalovirus must periodically undergo a blood test for anti-cytomegalovirus antibodies.
, Ganciclovir is the first antiviral drug historically approved for the treatment of Cytomegalovirus infections and represents the pharmaceutical preparation of "choice against the latter".
VALGANCICLOVIR
Administered orally, Valganciclovir can be associated with the use of Ganciclovir or replace the latter during the treatment of milder cytomegalovirus infections.
Important: Is It Possible to Cure Cytomegalovirus Infection in Pregnancy?
In the current state of science, the antiviral drugs available against Cytomegalovirus are not usable by pregnant women.
Therefore, a pregnant woman who develops Cytomegalovirus infection cannot take any medicines of those existing today and can only wait for the disease to take its course.
Important
Currently, there is no vaccine to prevent Cytomegalovirus infection in pregnancy.
However, research into the production of a vaccination is intense and has already provided extremely promising experimental results.