Definition of lichen planus
In the medical field, lichen planus identifies a chronic inflammatory dermatosis of immunological derivation, which mainly involves the skin and mucous membranes, but also the nails are often locus of pathological interest.

As can be guessed from the immunological nature of dermatosis, lichen planus is not contagious and appears in sensitive individuals when their immune system triggers an unjustified attack against the cells of the skin and mucous membranes.
The hallmark of lichen planus is the formation of papular lesions or itchy plaques, often erosive, with a relapsing course, but fortunately of a benign nature.
For further information: Lichen Planus Symptoms
Lichen planus is also known as 4P disease, depending on the typical clinical manifestations of the disease: Pruritic and Purple Polygonal Papules.
Term analysis
The term "lichen planus" derives from the typical manifestations of the disease, very similar to the arborescent formations of lichens. The very first description of lichen planus dates back to 1869, thanks to E. Wilson, who described the clinical evidence; dermatosis was also of interest to Kaposi, who focused on the bullous manifestations of lichen. Instead, in the first decade of the twentieth century, Darier described the complete histological clinical picture of lichen planus, analyzing, in the following years, also the variants dermatosis clinics. [excerpt from treatise on dermatology, lichen planus, F. Cottoni, M.A. Montesu].
Incidence
Lichen planus mainly affects women, but men are not totally excluded; interesting data emerged from medical statistics:
- lichen planus only rarely affects children;
- the oral form of liche planus occurs between 0.1 and 2.2% of cases;
- the favorite target of dermatosis are women between the ages of 50 and 70;
- infantile lichen planus is a rare variant: it seems to have a "high incidence in males of Indian ethnicity;
- the disease affects approximately 1% of the global population; in other texts, the "index of incidence" is more variable, estimated between 0.02% and 2%. Despite these uncertain data, it seems that in recent years the patients affected by lichen planus have been increasing slightly, probably thanks to the improvement of diagnostic techniques.
Causes
Many questions still need to be clarified about the etiology of lichen planus; however, it seems that in the light of recent studies, the genetic predisposition - correlated to peculiar environmental factors - has a significant impact on the manifestation of lichen planus.

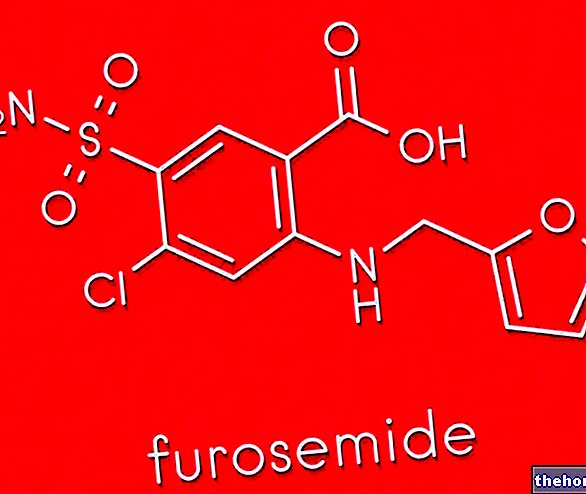
By examining the theories and the studies demonstrated by some authors, interesting possible conclusions emerged, useful to explain the etiology of lichen planus: biological, chemical and pharmacological factors could be possible causal elements, responsible for the antigenic alteration of keratinocytes, but also the anti-hepatitis B and flu vaccine, the abuse of NSAIDs, antihypertensives, anti-arthritics, Herpes simplex and hepatitis C could cause lichen planus, although these elements are questioned by many authors, because they are controversial.
Furthermore, it seems that smoking, dental amalgams, emotional stress and fungal infections (Candida albicans in particular) are other possible causal elements.
Cellular analysis of lesions
Following the manifestation of lichen planus, the cellular composition in the injured sites appears evidently altered: the basement membrane, characterized by an excess of fibrinogen, appears thickened, the epithelial crests tend to atrophy, the keratinocytes are destined for apoptosis. T lymphocyte infiltration is observed in the mucous membranes.
Classification
As we have seen, lichen planus can affect the skin and / or mucous membranes; according to the site of dermatotic manifestation and the evident clinical signs, the morbid disease is classified into several subcategories: anal-genital, cutaneous, nail, oral, and scalp lichen.
- Anal-genital lichen planus: a disorder that is observed mainly in women. Lichen planus generally causes vulvar itching and red skin, but the dermatosis could degenerate and cause an annoying burning sensation and pain in the internal vaginal mucosa, resulting in dyspareunia (possible pain during intercourse). In men, however, lichen planus (although not very frequent), could favor balanitis, postitis or balanoposthitis. The severe form is called sclero-atrophic lichen.
- Nail lichen planus: can affect the matrix or the nail bed. In the first case, the lamina appears thin, fragile with cracks ending in the free margin, presenting micro fragments: when not treated, the lichen planus at the level of the matrix causes a real destruction of the nail, with irreversible formation of dorsal pterygium (marked thinning of the proximal nail fold and cuticle, with evident scarring). If the nail bed is affected, the dermatosis could evolve in a negative direction and create hyperkeratosis and / or onycholysis. Most of the time, nail lichen planus causes brittle nails, which tend to flake and fall out.
- Cutaneous lichen planus: the papules appear pinkish-purple, with polygonal contours, albeit not well defined, covered by a shiny and hard to the touch surface. Generally, their diameter does not exceed 4-5 mm, but sometimes they can reach considerable dimensions (up to 2 cm in diameter). The papules created by lichen planus appear slightly desquamated, consisting of a sort of arboriform lattice, sometimes very itchy (hypertrophic lichen planus). Cutaneous lichen planus can occur in any superficial body site, especially in the back, forearms, legs, wrists and scalp.
In the palm plantar region, the papules appear rigid, yellow, hyperkeratotic: in general, the palmar-plantar lichen planus appears as callous ridges. - Oral lichen planus: inflammation of the internal mucous membranes of the mouth, which manifests itself with white or reddish spots, open wounds (sometimes bloody) and tissue swelling. In most cases, oral lichen planus lesions cause burning, pain or, more rarely, itching. It should be pointed out that oral lichen planus is not contagious, but more often than not it becomes chronic and also spreads to other body sites. Oral lichen planus, due to its variable localization and its heterogeneous clinical manifestations, is in turn divided into four subtypes: we speak of lichen atrophic when the preferred site is the lingual dorsum and generates an "evident atrophy of the lingual papillae, with consequent pain and burning when in contact with acidic foods.
Lichen reticular (more common and more easily diagnosed variant) manifests itself with white-pink reticular striae (striae of Wickham), of straight, dotted or arched type; it is frequently observed at the level of the lips, cheek, gum, lingual back: typical lateral lesions of the tongue, near the teeth. Again, lichen erosive occurs in the vicinity of the vestibular mucosa and lingual surface, characterized by painful ulcers, covered by a yellow film (erosive lichen of the ulcerative type) or by erythema at the level of the lingual mucosa (erosive lichen of the atrophic type), with consequent formation of papillae atrophic and whitish plaques. Lichen planus is sometimes misdiagnosed as discoid lupus and erythema multiforme. Finally, lichen planus a plate generates white plaques caused by the annexation of several hypertrophic papules (dorsal lingual): this disorder should not be confused with leukoplakia or candidiasis. - Lichen planus of the scalp: it is not uncommon for dermatosis to attack the scalp, generating hair loss (temporary or permanent alopecia) and possible scarring following the healing of the disorder. In the initial stage, lichen planus on the scalp begins with reddish papules, erythema, scaling, and follicular lichen (keratosis).
Other articles on "Lichen Planus"
- Lichen Planus: therapeutic strategies
- Lichen Planus - Medicines for the treatment of Lichen Planus
- Lichen Ruber Planus