The bronchial challenge test with Methacholine (TPBM) is a widely used test in the pneumological field, where it is used for the study of bronchial hyper-reactivity.
Bronchial Hyper-Reactivity
What does it mean?

This condition, typical of asthmatics, consists of an "abnormal broncho-constrictive response to various stimuli, which can be both internal (moods, emotions) and external to the body (allergens, cold and humid air, physical effort, viral infections).
When the organism is exposed to such stimuli, the respiratory tracts of a subject with bronchial hyper-reactivity tend to close with excessive ease and intensity. We speak of bronchial hyper-activity precisely because the same stimuli, at the same dose, do not cause responses. significant in healthy subjects.
Causes
In addition to asthmatics, an "excessive bronchial reactivity can also be recorded in obese subjects and in the last months of pregnancy.
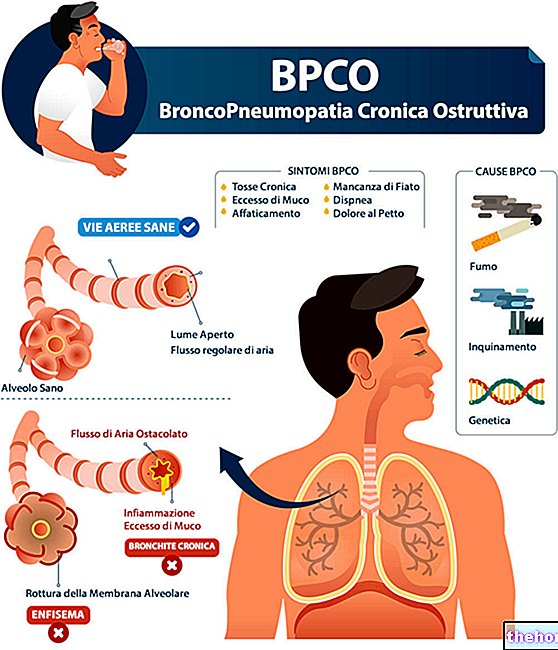
Hyper-reactivity is also characteristic of various diseases, such as COPD (chronic obstructive pulmonary disease), bronchiectasis, atopic dermatitis, allergic and non-allergic rhinitis, cystic fibrosis, heart failure and viral infections of the respiratory tract .
Employment in the study of asthma
The diagnostic significance of the methacholine test remains however mainly linked to the study of bronchial asthma.
Its wide use in clinical practice is given by the good reproducibility of the results and by the good safety, with low risk of systemic side effects (no fatal events or serious side effects related to the execution of the TPBM are reported in the literature). sensitivity, while considering the various and already listed possible causes of bronchial hyper-reactivity, the specificity of the methacholine test is moderate.
Ultimately, the methacholine test is a more useful test to rule out than to confirm the diagnosis of bronchaial asthma. In fact, the negative predictive value of the test is greater than the positive predictive value. In this sense, it is particularly useful when symptoms, spirometry and reversibility tests do not allow either to confirm or exclude the diagnosis. If the asthma is already known, the methacholine test instead helps to assess the severity of the asthmatic attack.
What principles is it based on?
The methacholine test exploits a particular characteristic of this substance. Methacholine is a synthetic muscarinic agonist of acetylcholine which, at the doses used in this test, is capable of triggering a small post-inhalation asthma crisis only in subjects with bronchial hyper-responsiveness. After its appearance, this crisis can be effectively controlled and resolved by administering an inhaled bronchodilator drug (spray or aerosol).
How is it done?
To evaluate and quantify the degree of bronchial reactivity, the test involves the aerosol administration of increasing doses of methacholine, followed, after each single inhalation, by spirometry.
The results of the latter are compared to those of the basal spirometry, performed before starting the test in order to evaluate any pre-existing bronchial obstruction.
A dose-response curve is thus obtained which expresses the degree of bronchial responsiveness of the subject. The lower the dose of methacholine capable of causing broncho-constriction, the greater the degree of bronchial hyper-responsiveness.
The test is stopped when the dose of methacholine administered causes a mild bronchial obstruction (evidenced by the reduction of 20% or more in the initial FEV1 - spirometric parameter), or after inhalation of the maximum expected dose. doctor intervenes by administering a bronchodilator drug (spray or aerosol).
Test preparation
Since bronchial hyper-reactivity can vary over time, increasing during exacerbations and decreasing during treatment with inhaled steroids, specific precautions should be taken before the methacholine test, such as the suspension of some therapies that may be in progress. Fasting it is not necessary, but before the bronchial challenge test with methacholine it is generally required to abolish smoking for at least 24 hours and together with it:
- tea, coffee, guarana, mate, coca-cola and other sources of caffeine for at least 24 hours
- Short-acting bronchodilators (eg Ventolin, Broncovaleas): for at least 8-12 hours
- Long-acting bronchodilators: for at least 24 hours
- Antileukotrienics (Montegen, Singulair, Lukasm, Zafirst etc.) for at least 24 hours
- Ipratropium bromide (Atem) - oxitropium for at least 24- 48h
- Tiotropium bromide (Spiriva) for at least 48h-1 week
- Antihistamines (eg Formistin, Aerius) for at least 72 hours
- Hormones - corticosteroids: for at least 4 weeks
- Medium duration of action theophylline (Theo Dur, Ansimar) for at least 24 hours
- Long-acting theophylline (Respicur, TheoNova) for at least 48 hours
PLEASE NOTE: Recommended withdrawal periods for individual medications may vary slightly depending on the medical center performing the methacholine challenge test.
While the aforementioned factors decrease the physiological response to methacholine, others amplify it; this is the case, for example, of exposure to allergens or sensitizers in the workplace, viral respiratory infections, atmospheric pollutants, cigarette smoke, of chemical irritants and B-blocking drugs.
Contraindications
The bronchial stimulation test with methacholine is contraindicated in the following cases:
- Recent heart attack or episodes of angina pectoris within the past three months
- Recent ischemia or cerebral hemorrhage (last three months);
- Known arterial aneurysm;
- Severe uncontrolled arterial hypertension: systolic> 200mmHg, diastolic> 100mmHg;
- Epilepsy in drug treatment;
- State of pregnancy or breastfeeding;
- Inability to perform spirometry correctly;
- Current use of cholinesterase inhibitors (used in the treatment of myasthenia gravis);
- Severe flow limitation: FEV1 <50% predicted or <1.0 L;
- Moderate flow limitation FEV1 <60% predicted or <1.5 L;





















-nelle-carni-di-maiale.jpg)




