Heart rate is one of the most important body parameters, because it is directly related to the vital function of the heart. It can increase or decrease to regulate blood circulation, in response to various types of stimuli or to perform physiological "compensations"; certain important modifications are instead interpreted as pathological symptoms.
Typical examples of "normal" heart rate variation are related to: physical activity, blood pressure, respiratory rate or release of hormone-neurotransmitters such as catecholamines. The physiological increase in heart rate is a way to deliver more blood, therefore more oxygen, to the tissues.
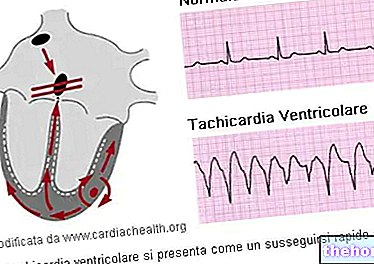
, even if this does not require special medical attention; furthermore it could be a problem, even if there are many athletes with less than 50 bpm without any symptoms or uncomfortable conditions. Between 90 and 100 the value is still considered normal, but persistent rates between 80-100 bpm, especially during sleep, can be signs of hyperthyroidism or anemia. In addition to 100 bpm we speak of tachycardia.
A "high resting heart rate is associated with an increase in cardiovascular and all-cause mortality in the general population and in patients with chronic disease. A faster resting heart rate is therefore associated with a shorter life expectancy and is considered a strong risk factor for heart disease and heart failure, regardless of physical fitness level. A resting heart rate above 65 bpm has been shown to have a strong, albeit independent, effect on premature mortality; a 10 beats per minute increase in HR at rest has been shown to be associated with a 10-20% increased risk of death. Men with no evidence for heart disease and a resting heart rate of over 90 bpm have a five times greater risk of sudden cardiac death. Men with a resting heart rate of over 90 bpm have an almost double increased risk of mortality from cardiovascular disease; in women the increase is even triple.
Lifestyle changes and drug therapies can be helpful in decreasing high resting heart rates. Exercise is a potentially useful measure and one to consider when an individual's resting heart rate is above 80 bpm. Diet has also been shown to be beneficial in lowering resting heart rate: in HR studies at rest and the risk of death and heart complications in patients with type 2 diabetes, consumption of legumes has been shown to reduce resting heart rate. This is thought to happen because, in addition to having direct beneficial effects, these foods affect reducing saturated fat and cholesterol.
Regardless of individual predisposition, aerobic sport practiced for many years and with heavy workloads tends to reduce HR, both at rest and during activity. On the contrary, high intensity disciplines (HIT) allow to maintain the ability to reach very high beats per minute in maximal and submaximal efforts.
Resting heart rate can also be affected by certain medications; for example, stimulants such as amphetamines tend to increase it, while sedatives and antidepressants help reduce it.
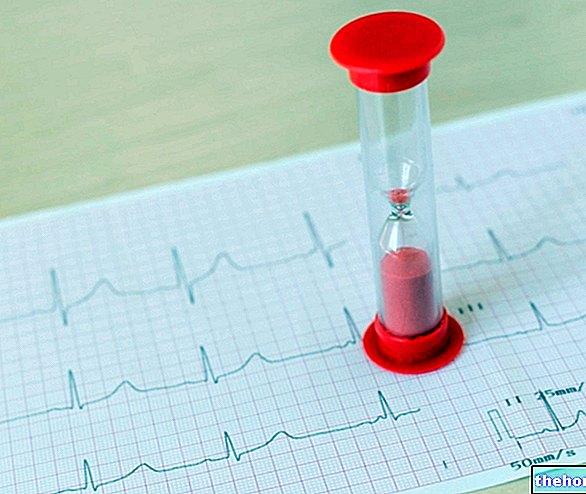
Heart rate is measured both at rest and during exercise, depending on the investigation to be carried out; while the former is an integral part of any basic medical examination, the latter case is particularly referred to the control for competitive sports fitness. .
cardio accelerators
Factors that reduce heart rate and force of contraction
The simplest method is the instrumental one, as it minimizes operator-dependent error.
Devices that allow you to measure the heart rate at rest are: heart rate monitor (chest or wrist), pulse oximeter, electronic sphygmomanometer (not manual, which instead requires specific skills of use) and stethoscope.
The electrocardiogram also performs this function, however dedicated to more complex diagnostic investigations, generally carried out in the health sector and by competent personnel.
How to measure resting heart rate without heart rate monitor?
The measurement of the heart rate at rest is carried out by palpating the radial artery (on the wrist) or the carotid artery (on the neck), feeling the change in pressure on the fingertips. The ideal time span is a full minute, during which it is necessary to count the beats accurately. It is good to remember that the applied force must be light, especially in correspondence with the carotid artery.
Alternatively, it is possible to detect the pulsations in a segmented way, for example every 10, 15 or 20 seconds, noting them in a table and extrapolating the final value at the end (by multiplying x 6 in the first case, x 4 in the second and x 3 in the third).