What it is and why it is performed
The urea breath test is a simple, non-invasive and highly accurate diagnostic test, widely used in gastroenterology for the diagnosis of Helicobacter Pylori infection.

Helicobacter Pylori
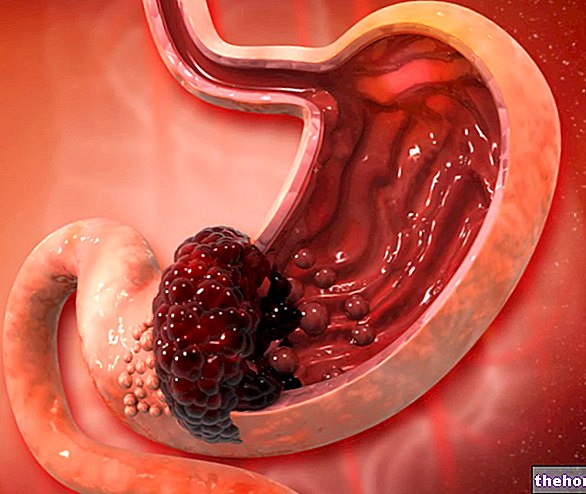
This microorganism is considered the only bacteria capable of resisting the acidity of the gastric environment, to the point that it sneaks into the gastric mucosa and replicates there; this characteristic is conferred by the strong ability to produce urease, an enzyme that breaks down urea in the stomach releasing carbonic acid and ammonia; in this way, the urease neutralizes the gastric acids creating a microenvironment favorable to the replication of the bacterium.
The growth of Helicobacter Pylori brings with it a series of unpleasant consequences for the patient, predisposing him to gastritis, stomach ulcer and, in some cases, stomach cancer. The doctor can then prescribe the urea breath test in case the subject complains of persistent gastric symptoms, attributable to hyperacidity, gastritis or gastroduodenal ulcer. Moreover, thanks to the excellent specificity and sensitivity of the test, the urea breath test can be repeated over time to monitor the efficacy of medical therapy undertaken to eradicate Helicobacter pylori infection.
How does it work
The breath test uses the high urease activity of Helicobacter pylori to diagnose infection.
Conceptually rather simple, the test is based on the administration of urea labeled with a carbon isotope (13C or 14C); once ingested, the urease produced by the bacteria hydrolyzes urea into ammonia and carbon dioxide, which is absorbed by the gastric walls, then carried by the blood and rapidly excreted in the exhaled air.
For what has been said, in the presence of a "gastric infection by Helicobacter Pylori, we will find a certain amount of radiolabelled carbon dioxide in the air exhaled by the patient after a few minutes from the start of the test. Analyzing this" air using special instruments we go back to ratio between the isotope of the carbon chosen to label urea and 12C, the most frequent in nature. In general, currently, it is preferred to use the isotope of carbon 13C as a marker of urea, as it is stable, present in nature, non-radioactive and harmless (unlike 14C which is radioactive, to a slight but not negligible extent, at point to make subjecting to too close breath tests contraindicated).
In the healthy subject there is no urease activity in the stomach due to the absence of the bacteria; therefore the urea administered by the test is absorbed and eliminated in the urine.
The specificity of the urea breath test is 100% and its sensitivity is also close to the maximum values (97%). The test can give false negative results when carried out shortly after therapies with drugs that inhibit metabolic activity and urease of the bacterium of the bacterium (antisecretors) In these cases, the negativity of the test could mean only a momentary inhibition of the bacterium (clearance) and not the complete and definitive elimination (eradication).
How to Perform the Exam
The urea breath test is generally performed in the morning, after fasting for at least 6 hours.
We proceed with the sampling of the basal exhaled air (before taking the Urea): the patient is invited to make a deep inhalation and to blow through a straw for drinks into a vial, completely exhaling the air contained in the lungs; the patient immediately delivers the vial to the operator, who immediately closes it. The entire procedure is then repeated in a second tube.
At this point, the patient is invited to drink a 13C marked urea solution, and to wait thirty minutes sitting in the waiting room without drinking, eating or smoking. At the end of half an hour, the patient repeats the previous operations: using a straw for drinks, blows again into a first tube (time 30 minutes), completely emptying the lungs; hands the tube to the operator who plans to seal it, then repeats the procedure with a second tube.
The exhaled air is analyzed by mass spectrometer, which allows to measure the amount of CO2 with 13C compared to the total exhaled CO2. As anticipated, in the presence of Helicobacter pylori in the stomach, an increase of 13C in the exhaled air is determined, hence an increase in the ratio between 13C and 12C.
Preparation
Preparation for the exam provides - unless otherwise indicated by a medical practitioner - abstention:
- for three weeks after use of associated antibiotics and proton pump inhibitors (use of a single antibiotic does not appear to interfere with the test):
- for one week from the use of gastroprotective drugs belonging to the class of proton pump inhibitors or H2 antagonists, in addition to sucralfate (therefore pharmaceutical specialties containing cimetidine, ranitidine, pyrenzepine, nizatidine, lansoprazole, rabeprazole, pantoprazole, omeparazole, esomeprazole are to be avoided , sucralfate, of which a list follows: antepsin, antra, axagon, biomag, brumethidine, buscopan antacid, citimid, citronizat, controloc, crafilm, cronizat, dina, ermes, esopral, etideme, eugastran, eureceptor, famodil, frilans, gastr gastridin, gastrogel, lansox, leblon, levogenix, limpidex, lomevel, losec, lucen, mepral, motiax, nansen, neoh 2, nexium, nizax, notul, omeprazen, pantecta, pantoloc, pantopan, pantorc, pariet, peptazol, peptidirex, pergastridirex , raniben, ranibloc, ranidil, ranidiz, roxit, sensigard, stomet, sucralfin, sucramal, sucrate, sucroril, suril, tagamet, temic, ulcedin, ulcestop, ulcex, ulcodina, ulcomedina, ulcrast, ulis, zanizal, zantac, zoton). Consult your doctor for further and more precise indications.
On the day of the breath test, the patient must have been in the laboratory fasting for at least 6 hours if an adult, 3 if a child. It is also important to refrain from smoking and coffee in the morning before the exam.
Risks and Complications
The Urea Breath Test for the diagnosis of Helicobacter Pylori is completely painless and lasts an average of thirty minutes. For non-invasiveness, the examination is free from complications and risks.