Definition
Sarcoidosis reflects a pathological condition in which the formation and development of small clusters of inflamed cells (granulomas) is observed in different body sites; normally, sarcoidosis affects cells in the lungs, lymph nodes, eyes, and skin, but it can ideally spread to any anatomical area.
Causes
To date, a definite and precise cause responsible for sarcoidosis has not yet been identified; however, in some patients there is a marked genetic predisposition to the disease, triggered, in turn, by exposure to viruses, bacteria or other chemicals. What is certain is that in sarcoidosis some cells of the immune system go mad and become they aggregate, forming inflamed cell clusters.
Symptoms
Symptoms depend on the anatomical site affected by sarcoidosis, although fever, weight loss and loss of appetite are common signs for most forms of sarcoidosis.
- Pulmonary sarcoidosis → dyspnoea, hemoptysis, shortness of breath, cough
- Sarcoidosis of the lymph glands → enlargement and swelling of the lymph nodes in the neck, arms, chest
- Sarcoidosis of the skin → alteration of the skin color (purplish), erythema nodosum, skin rash raised on the face
- Renal sarcoidosis → kidney stones, hypercalcemia
- Hepatic and splenic sarcoidosis → hepato / splenomegaly
- Sarcoidosis of the heart → cardiomyopathy, heart failure, cardiac irregularities (e.g. bradycardia)
- Ocular sarcoidosis → visual impairment, uveitis
- Joint / muscle sarcoidosis → pain, inflammation
- Sarcoidosis of the nervous system → visual impairment, hearing impairment, meningitis, swallowing problems
Information on Sarcoidosis - Sarcoidosis Treatment Drugs is not intended to replace the direct relationship between health professional and patient. Always consult your doctor and / or specialist before taking Sarcoidosis - Medicines to Treat Sarcoidosis.
Medicines
Overall, the symptoms accompanying sarcoidosis are not particularly severe; since the statistical data reveal that 75% of patients do not complain of severe symptoms, the administration of drugs is reserved for very few patients, as well as for those cases in which sarcoidosis generates imbalances such as to interfere with normal daily activities.
However, in the case of a diagnostic finding even in the absence of symptoms, it is recommended to undergo regular medical checks to, if necessary, intervene before the disease progresses, creating damage; among the most recurrent diagnostic tests, we mention the chest X-ray, the control of lung function and the outpatient visit.
Medical-pharmacological treatment becomes essential in case of confirmed cardiac, pulmonary and other vital organ involvement.
The main goal of medical therapy is to reduce inflammation, followed clearly by the reduction of pain and the removal of secondary symptoms (when present). The most widely used drugs are corticosteroids which, as we know, cannot be used for long periods because of the consistent side effects that can induce, even NSAIDs can be taken, especially when the pain and inflammation associated with sarcoidosis are mild or moderate, however bearable.
If sarcoidosis involves more pronounced symptoms, a more powerful specific therapy is conceivable: anti-rejection drugs (used for suppressing the immune system), inhibitory drugs of tissue necrosis factor alpha (for sarcoidosis associated with rheumatoid arthritis) and drugs antimalarials (for the treatment of cutaneous sarcoidosis involving the nervous system).
Rarely, sarcoidosis cannot be cured only with drugs: some forms, particularly aggressive, require a lung or heart transplant, or a peacemaker to coordinate the heart rhythm.
The following are the classes of drugs most used in the therapy against sarcoidosis, and some examples of pharmacological specialties; it is up to the doctor to choose the most suitable active ingredient and dosage for the patient, based on the severity of the disease, the state of health of the patient and his response to treatment:
NSAIDs for the control of mild pain associated with sarcoidosis: non-steroidal anti-inflammatory drugs are used in therapy to mask mild pain in the context of sarcoidosis, while exerting a moderate anti-inflammatory effect. The following are the most used drugs:
- Ibuprofen (eg. Brufen, Moment, Subitene): for medium-moderate pain, it is recommended to take by mouth a dose of active equal to 200-400 mg (tablets, effervescent sachets) every 4-6 hours after meals, at need. Do not take more than 2.4 grams per day.
- Naproxen (eg Aleve, Naprosyn, Prexan, Naprius): it is recommended to take the drug at a dosage of 550 mg, orally, once a day, followed by 550 mg of active ingredient every 12 hours; alternatively, take 275 mg of naproxen every 6-8 hours, as needed. Do not exceed 1,100 mg per day.
- Paracetamol or acetaminophen (eg Tachipirina, Efferalgan, Sanipirina, Piros, Tachidol): the drug is NOT an anti-inflammatory; however, it is still indicated in the context of sarcoidosis to reduce pain and fever. Paracetamol is administered at a dosage of 325-650 mg per day every 4-6 hours; alternatively, take 1 gram every 6-8 hours. The dosage depends on the patient's condition, age and weight.
Corticosteroids for the treatment of sarcoidosis
Steroid drug therapy is recommended when sarcoidosis occurs in the lung (to be taken in the form of a nasal spray), joint, skin, nerve, and heart (in the form of tablets or injections).
In the form of eye drops, medications can also be instilled into the eye if the granulomas obscure vision.
Medical statistics show that after stopping steroid therapy, sarcoidosis tends to relapse; to overcome this inconvenience, an additional therapy (lasting 2-3 months) is sometimes recommended as a prevention to relapse from sarcoidosis.
- Prednisone (eg Deltacortene, Lodotra): the dosage should always be established by the doctor based on the severity of the sarcoidosis and the patient's condition. Indicatively, the dose to be taken varies from 5 to 60 mg per day, possibly divided into several doses (1-4) over the course of 24 hours. Generally, the most effective dosage seems to be between 15 and 20 mg per day. .
- Methylpredinone (eg Medrol, Urbason, Advantan, Depo-medrol, Solu-medrol) it seems that most patients with sarcoidosis respond positively to treatment with methylprednisone at a dose of 12-16 mg / day. In very severe cases, it is possible to increase the dose up to 48 mg per day.
- Triamcinolone (eg. Kenakort, Triamvirgi, Nasacort): the drug is particularly indicated for sarcoidosis with pulmonary involvement. As a guideline, take 16-48 mg orally, once a day. It is recommended to strictly follow the doctor's instructions.
- Dexamethasone (eg Decadron, Soldesam): the drug is used in therapy for sarcoidosis as a second choice. For the posology: consult your doctor.
- Cortisone (eg. Cortis Acet, Cortone): for the treatment of sarcoidosis, the indicative dosage is to take 25-300 mg per day of the drug, orally, intramuscularly, in one or two doses per day. Consult your doctor.
It is recommended not to use corticosteroids for long periods: prolonged use can lead to weight gain, mood swings, osteoporosis, lethargy, liver and blood cell damage, petechiae / bruising, hypertension, increased risk of diabetes, thinning of the skin.
Anti-rejection drugs for the treatment of sarcoidosis: the objectives to be achieved in case of severe sarcoidosis are both to suppress the immune system and to reduce inflammation. This therapy is normally recommended when a treatment based on steroid drugs has not brought the desired therapeutic effects.
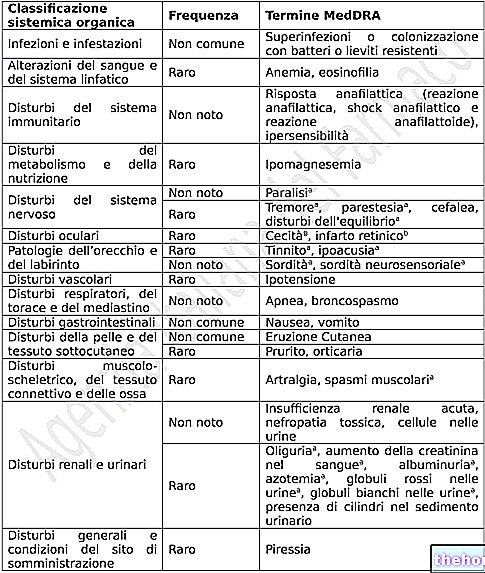
It should not be forgotten that the administration of these active ingredients can make the subject more vulnerable to infections.
- Methotrexate (eg Reumaflex, Methotrexate HSP, Securact): the drug is an antagonist of folic acid synthesis, capable of heavily influencing the body's immune response. In this regard, it is widely used in the treatment of sarcoidosis. Initiate therapy - in sarcoidosis patients unresponsive to corticosteroid drug therapy - with a low dose of 2.5 mg / week. It is possible to gradually increase the dosage (by 2.5 mg / week), up to a maximum of 10-15 mg / week. Some patients require the combination of methotrexate + corticosteroid
- Azathioprine (eg Azathiopirine, Immunoprin): immunosuppressant drug of the immune system, indicated in the treatment of sarcoidosis to reduce the administration of corticosteroids. Begin therapy with a drug dose of 2mg / kg per day, in combination with 0.6-0.8 mg / kg of prednisone; after 2-3 months of treatment, the dose of prednisone taken can be reduced to 0.1 mg / kg. The maintenance dose suggests taking 2 mg / kg of drug per day with prednisolone (0.1 mg / kg / day) for long periods (21-22 months).
Antimalarial drugs for the treatment of sarcoidosis: indicated for the treatment of sarcoidosis with evident involvement of the skin and nervous system, especially when moderate or severe hypercalcemia is observed in the patient. When prolonged, therapy with these drugs can induce eye damage.
- Hydroxychloroquine (eg. Plaquenil): the antimalarial drug is indicated for the treatment of mild rheumatoid arthritis in the context of sarcoidosis. The dosage suggests taking 200 mg of the drug per day: this dosage proved to be more useful than corticosteroids, especially for cutaneous forms of sarcoidosis.
Tissue necrosis factor alpha inhibitor drugs: indicated for the treatment of sarcoidosis in patients with rheumatoid arthritis.Excessive / prolonged use with these drugs can promote lymphomas, blood diseases and congestive heart failure.
- Infliximab (eg Remicade): latest generation drug capable of arresting the action of molecules involved in the inflammatory process that distinguishes sarcoidosis. The dosage involves taking 5mg / kg of drug, by intravenous infusion to be repeated at the second, fourth and eighth week from the first injection given for the treatment of sarcoidosis.
Other articles on "Sarcoidosis - Drugs to Treat Sarcoidosis"
- Sarcoidosis: symptoms, diagnosis and therapy
- Sarcoidosis