Index Article
Acute pancreatitis is manifested by a sudden and violent pain in the upper part of the abdomen, the anatomical seat of the pancreas, with a tendency to radiate towards the back. The painful symptoms typically worsen after meals, with deep inhalations and during palpation of the abdomen; instead they tend to be relieved by bending forward (the patient searches for and maintains an analgesic position). The pain is often followed by nausea and vomiting food and biliary (green - dark color), while the patient is particularly suffering, febrile, anxious and agitated, often with signs of shock (cold and pale skin, marked hypotension, small and frequent pulse). pain, often however resistant to drugs, reaches its maximum progressively, remains intense for a long time and gradually decreases over the course of days or weeks.
In chronic pancreatitis the symptoms are more nuanced, so much so that sometimes the inflammation develops in a paucisymptomatic manner; the patient complains of pain in the upper part of the abdomen, associated with an "inexplicable weight loss, lack of appetite and digestive difficulties with appearance of steatorrhea (greasy, greasy stools, especially in conjunction with copious meals with a high lipid content).
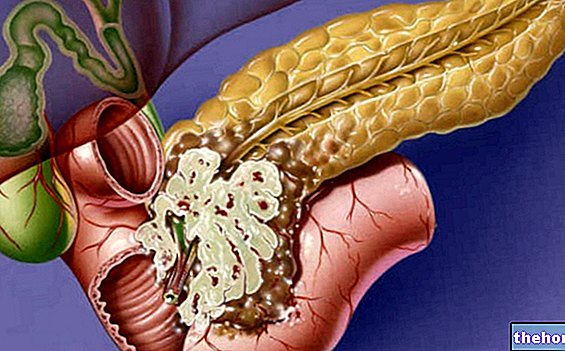
pancreatic, especially proteases, are synthesized in an inactive form, in order to protect the cells that produce them from their damaging action. When these enzymes, transported by the pancreatic juice, pour into the duodenum (initial section of the small intestine) they undergo an activation process, which is necessary for the optimal performance of digestive activities. In pancreatitis, the inflammatory process affecting the pancreas is sustained precisely by the early activation of these enzymes within the gland. Repeated insults can therefore cause chronic damage to the pancreas (self-digestion, necrosis of the vessels and consequent inflammatory reaction), with gradual loss of its functionality, in these cases we speak of pancreatic insufficiency Unfortunately, the reduced function of the pancreas causes serious digestive problems and poor glycemic control, with the onset of diabetes.
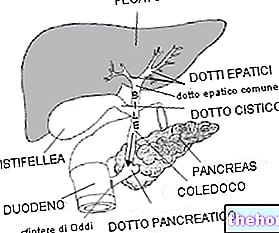
There are numerous, and often associated, possible causes of pancreatitis; among the most common we remember gallstones, in which one or more "pebbles" migrate from the gallbladder or biliary tract into the "ampulla of Vater (dilation of the choledochus in which the pancreatic juices transported by the bile duct join the bile, coming from the liver and from the gallbladder, for a very short distance, before pouring into the duodenum). An obstruction at this level prevents the normal outflow of bile and pancreatic juice into the intestine; consequently, these secretions tend to rise up and accumulate inside of the gland, causing and supporting the inflammatory process. For the same reason, pancreatitis is typically caused by inflammation or malfunctioning of the sphincter of Oddi (a muscle ring located downstream of the ampulla of Vater, which tends to let digestive juices flow freely after a meal and to hinder them. during fasting, when their action is no longer necessary). Obstructive processes at various levels can also be favored by "hyperparathyroidism and" hypercalcemia, which facilitate the activation of enzymes within the pancreas and the appearance of calcifications of the ductal excretory system and pancreatic parenchyma.
Another rather common cause of pancreatitis is alcoholism (ductal hypertension and edema), especially when it is aggravated by other unhealthy habits, such as smoking (smoking) or a habitually hyperlipidic and hyperproteic diet. Not surprisingly, attacks of acute pancreatitis often occur following a heavy meal or conspicuous ingestion of alcohol. Hypertriglyceridemia is also an important risk factor for pancreatitis, together with the inevitable family predisposition and some drugs (such as azathioprine, thiazide diuretics, asparaginase, estrogens, tetracyclines and corticosteroids).
The less common causes include cystic fibrosis, violent abdominal trauma, tumors of the pancreas or sphincter of Oddi, penetrating duodenal ulcer, viral infections, surgical interventions involving nearby organs (stomach, biliary tract, duodenum , spleen) and an interventional diagnostic procedure called retrograde endoscopic cholangiopancreatography.
In a not negligible number of cases it is not possible to identify any cause of origin; in these cases we speak of idiopathic pancreatitis.
Pancreatitis: Symptoms, Diagnosis, Treatment and Prevention
- Go to the Video Page
- Go to Wellness Destination
- Watch the video on youtube
Other articles on "Pancreatitis"
- Pancreatitis: diagnosis, care and treatment
- Pancreatitis - Medicines for the treatment of pancreatitis
- Pancreatitis diet