Diagnosis
For a correct clinical diagnosis, the dermatologist must visit all visible skin and mucous membranes with the patient completely undressed and with adequate lighting.In particular, it is also necessary to carefully observe places that the patient hardly observes alone, such as the spaces between the fingers (interdigital), the soles of the feet, the hair, the nails, the auricular regions, the perianal region and the genitals. .
Through a tool called dermoscope, the dermatologist can see the lesion enlarged about 10 times or, through another instrument called operating microscope, up to 60 times, after making the stratum corneum transparent by applying a particular oil on the skin surface. This allows to study pigmented structures present in the epidermis and dermis and, above all, to distinguish a malignant lesion from a benign one. .
In the case of a suspected melanoma, the entire lesion must be removed but with healthy skin margins that do not exceed 3 millimeters. This technique is called excisional biopsy. A histological examination under an optical microscope will be carried out on the removed lesion and, once the diagnosis is histologically confirmed, a new radical intervention will have to be carried out as soon as possible, within the maximum limit of 30 days from the execution of the biopsy.
What is defined instead incisional biopsy, ie the removal of a part of the lesion for diagnostic purposes, as a rule should not be performed because there is a risk of disseminating tumor cells. Few exceptions are allowed, that is, when clinical doubt remains and when the excisional biopsy would otherwise involve complex or too much demolitive, for example when the lesion is in the subungual area (under the nail), or is a giant congenital nevus or a large lentigo of the face.
Finally, to define the anatomical extension of the disease, a chest X-ray and a liver ultrasound (to evaluate any metastases) should be performed. Further and more complex tests, such as abdominal and pelvic and cerebral CT scans, will be performed only in the presence of a precise clinical doubt.
As regards the diagnostic confirmation of a lymph node suspected of being the site of metastases, needle biopsy with a fine needle is now considered a technique of choice (fine needle aspiration) with the cytological examination of the aspirate.
Surgical therapy
The purpose of surgical therapy on primary melanoma is to radically remove the tumor; relapse during surgery, if the technique is correct, is absolutely rare (less than 5%). The tumor must be removed with a border of healthy skin and the excision must also include the subcutaneous tissue reaching up to the muscle fascia, which is not normally removed. The width of the healthy skin margin foresees excisions at 1 centimeter for thick melanomas less than 2 millimeters and 2-3 centimeters for thicker lesions.
Surgical therapy of lymph node metastases involves the cervical, axillary and inguinal lymph nodes.
For melanomas with a maximum thickness greater than 1 millimeter, selective lymph node dissection based on the outcome of the sentinel lymph node biopsy is now routine. The technique consists in injecting 1-2 milliliters of dye and / or a radioactive substance in the vicinity of the tumor or scar that remains after the biopsy and to carry out a biopsy of the first one immediately afterwards
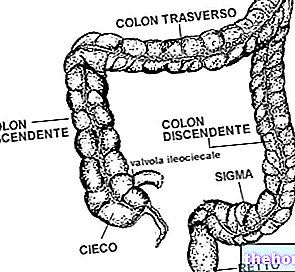
Surgical therapy of distant metastases should be performed only when they are easily accessible (skin and subcutaneous, gastrointestinal tract), but only with the aim of extending the patient's life and relieving the symptoms (palliative purpose).
Medical therapy
He uses chemotherapy, which is used only in advanced stage (stage IV) melanoma. Regional chemotherapy (by hyperthermic-antiblastic fusion) inside the dermis is indicated in cases of localized melanoma in the limbs and in the presence of local and regional skin metastases.
Radiotherapy involves the use of very high doses of rays, as only in this way the tumor becomes radiosensitive.
Sentinel Lymph Node Technique
This technique is a fundamental diagnostic moment not only with regard to cutaneous melanoma, the first tumor that has seen its application used, but also for other neoplasms, such as those of the breast for example.
The sentinel lymph node is the first tributary lymph node of the tumor; this means that it is the very first lymph node that receives the lymph coming from the cutaneous area where the tumor originated. It is almost always unique, but two or sometimes three may be present, in the same region or in distinct regions.
This technique aims to see whether or not there are micrometastases in the lymph node itself and this can only be seen by identifying it, removing it, and making many sections or "slices". If the sentinel lymph node is positive, that is, it has tumor micrometastases, the other lymph nodes that follow it will most likely be positive as well, and therefore all of them will be removed en bloc; if it is negative, inevitably, being the first, all the others must necessarily be negative.
The technique is used only if the melanoma has a diameter equal to or greater than 0.76 millimeters. For smaller diameters, it can be confidently stated that the tumor has not yet given any metastases to the lymph nodes.
Initially, the technique consists of "identifying the lymph node by injecting a dye labeled with radioactive technetium into the dermis at the edges of the melanoma or its surgical excision scar and performing an instrumental examination called lymphoscintigraphy which will identify the first lymph node in which the radioactive dye is distributed. Once identified, the same lymph node is surgically removed and sent to the pathologist, who will study it by making many sections and seeing if, in each of these, a microscopic tumor metastasis may be present. If the lymph node is positive for micrometastasis, it is removed surgically all the lymph node package, that is all the lymph nodes near and downstream the sentinel, which communicate with him, those of the sentinel's tributary chain. A complication of all this is the edema (dermal and subcutaneous fluid effusion) that follows, which is the main side effect of an "removal of this kind.
Other articles on "Melanoma - Diagnosis and Treatment"
- Melanoma classification
- melanoma
- Melanoma - Medicines for the treatment of Melanoma