Transperineal biopsy
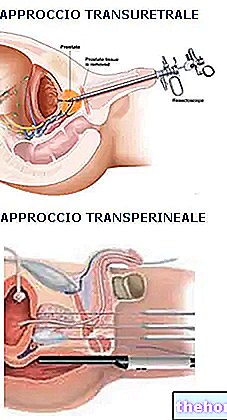
During the transperineal prostate biopsy, the patient lies in the supine position, with the thighs flexed towards the chest and with one hand supporting the scrotum.
After a preventive rectal exploration, the ultrasound probe is inserted via the anus, similar to that described for the transrectal biopsy approach. The perineum, that is the area between the scrotum and anus, is adequately depilated and disinfected; in this area a double dose of anesthetic, the first in the superficial layers and the second, after a few minutes, deep in the tissues surrounding the prostate.

After a further wait, a very thin hollow metal canal is then inserted into the perineum, inside which the biopsy needle slides easily, saving the patient the hassle associated with repeated passage of the same.
The tissue samples taken during prostate biopsy, called frustules, are subsequently examined under an optical microscope by the pathological specialist, who within a few days draws up the histological report of the examination. The microscopic analysis allows to distinguish healthy cells from cancerous ones. and, in the eventuality, to establish the localization and the degree of abnormality and aggressiveness of the same. For this purpose a numerical scale (Gleason score) is used which goes from one + one (slight degree of abnormality) to five + five ( maximum degree of anomaly with high probability that the tumor will develop and spread rapidly). In the case of abnormal cell findings, but not necessarily cancerous, a second biopsy is usually required (after three / six months) in order to ascertain the absence of ongoing tumor processes.
Risks
Is the exam painful?
Thanks to the use of anesthetics, prostate biopsy is generally well tolerated and not very painful. Very short pangs of limited intensity are typically felt during biopsy sampling.
What are the possible complications?
Be that as it may, prostate biopsy remains an invasive diagnostic procedure and as such burdened by a series of risks related to the type of anesthesia, the age of the patient and his general condition.
Specifically, prostate biopsy can give hemorrhagic, inflammatory, infectious and allergic complications.
Bleeding complications
Hemorrhagic complications are the most frequent, so much so that up to 20% of cases occur; in general these are light and transient bleeding, made evident by more or less conspicuous traces of blood in the urine, faeces and / or ejaculate; in this sense it is not even correct to speak of complications, given that within certain limits they are to be to be considered normal phenomena. Urinary haemorrhage rarely becomes conspicuous, to the point of forming large and consistent clots that occlude the urethra, preventing the bladder from emptying, with consequent inability to urinate. This eventuality requires catheterization and bladder emptying. at the nearest emergency room, it can be prevented by drinking plenty of water after surgery. Traces of blood can also be evident in the stool during evacuation, but only when the prostate biopsy is performed transrectally; also in this case, within certain limits, it is a fairly common and not worrying event that can continue for a few days; only when the bleeding persists over time, or becomes particularly conspicuous, a prompt medical intervention is necessary. Finally, very importantly, after a prostate biopsy, the bleeding often becomes evident during the first ejaculations. consequently, it abandons the classic whitish and opalescent reflections to take on dark, "coffee milk" shades; also in this case the situation spontaneously returns to normal within a few weeks.
Furthermore, in individuals subjected to transperineal prostate biopsy, the formation of a hematoma in the access area of the biopsy needle, located between the scrotum and the anus, is common; once again, if the hematoma and swelling become particularly consistent, it is advisable to alert your doctor as soon as possible.
Let's now look at some terms used by doctors in relation to the possible complications of prostate biopsy:
- hematuria (presence of blood in the urine, which can be minimal - microhematuria - or conspicuous - macrohematuria);
- hemospermia (presence of blood in the sperm);
- rectal bleeding (rectal bleeding);
- phlogosis (synonym of inflammation).
Other articles on "Prostate Biopsy - Reliability and Complications"
- Prostate biopsy
- Preparation for prostate biopsy

.jpg)