Generality
MRSA is a human bacterial infection caused by strains of Staphylococcus aureus particular, as they are resistant to some antibiotics such as penicillins and cephalosporins.

Figure: Methicillin-resistant Staphylococcus aureus seen under a scanning light microscope (artificial staining).
The disease mainly affects people admitted to hospitals; however, in recent years, it is spreading more and more even among non-hospitalized people, especially among those who spend a lot of time in close contact with other individuals (prisoners, athletes of sports teams, students, etc.).
The symptoms are extremely variable: MRSA, in fact, can manifest itself not only with boils, abscesses and infectious cellulitis, but also with fever, chills, septicemia, endocarditis, etc.
Therapy depends on the characteristics of the infection and the results of the culture tests.
What is MRSA?
MRSA is a human bacterial infection caused by particular strains of Staphylococcus aureus, resistant to β-lactam antibiotics such as penicillins (methicillin, dicloxacilin, nafcilin, oxacilin, etc.) and cephalosporins.
WHAT IS THE RESISTANCE OF BACTERIA TO ANTIBIOTICS DUE TO?
Bacteria become resistant to an antibiotic when they accidentally develop a genetic mutation that leads them to survive the bactericidal action of the drug. For example, they may acquire a defense mechanism they did not previously have.
The great diffusion of antibiotic-resistant bacteria, which took place in recent decades, is linked to the "indiscriminate use that has been made of antibiotics: with their abuse, in fact, susceptible bacteria have been exterminated and the resistant ones (who were in minor number) to acquire dominance within the species.
MEANING OF MRSA
MRSA is the acronym for Staphylococcus Aureus Methicillin resistant. This acronym (which in the light of the definition given may seem unsuitable) was coined because the first antibiotic, to which some strains of Staphylococcus aureus, it was methicillin.
When biologists and doctors realized that the resistance of these strains was also directed towards the other penicillins and cephalosporins, the term MRSA had by now entered the common jargon and was never changed.
What are MSSAs?
Staphylococci aurei not resistant to penicillins and cephalosporins are classified with the abbreviation MSSA, or Staphylococcus Aureus Sensitive to Methicillin. Even for these, the acronym that identifies them does not fully reflect their characteristics; however, it has now entered into common use and has been maintained as such.
STAPHYLOCOCCUS AUREUS
The Staphylococcus aureus it is a gram-positive bacterium, spherical and asporigenous, which colonizes mainly the nasopharyngeal mucous membranes, the skin and the cutaneous glands. The infection it causes can be minor if limited to the skin (impetigo, abscesses and boils), but it can also be fatal if it passes through the skin and spreads to the blood or heart.
TYPES OF MRSA
The first cases of MRSA have occurred since the early "60s of the last century and, for at least twenty" years, have concerned only hospital patients.
In the early 1980s, even non-hospitalized individuals began to contract the infection. Most affected were people in extremely crowded places, such as prisons, homeless shelters, student dormitories, gym and sports field locker rooms, barracks and schools.
The site of infection, therefore, was taken as a parameter to distinguish two types of MRSA:
- HA-MRSA, where HA stands for Healthcare-Associated and refers to all cases of MRSA who became infected during a hospital stay.
- CA-MRSA, where CA stands for Community-Associated and refers to all cases of MRSA that have contracted the infection outside of a hospital and usually in a crowded location.
Although the number of cases of CA-MRSA is soaring today, HA-MRSA is still the most prevalent type of MRSA.
Causes
The bacterium responsible for MRSA is usually transmitted by direct contact, for example through the hands of an infected or colonized individual (NB: by colonized individual, we mean a person capable of spreading a pathogen, but, despite this, healthy). Other ways of transmission are represented by the so-called skin-to-skin contact and by everything that has been previously touched by an individual with MRSA (for example towels, sheets, clothes, etc.).
MRSA is very durable and is capable of surviving on the surface of objects (doorknobs, sinks, floors, etc.) for long periods of time.
HA-MRSA
MRSA has been, and continues to be, a typical infection in hospital settings for at least three reasons:
- The presence of wounds that represent entry points for the bacterium. Often, hospital patients are people with injuries (fortuitous or post-surgery) or catheterized (ie with bladder or intravenous catheters); this means that it is easier, for a bacterium such as MRSA, penetrate inside the organism and trigger the homonymous infection.
- The fragility of hospitalized patients. In hospitals, a high percentage of inpatients are elderly or immunosuppressed (ie with reduced immune defenses). Seniority and the lack of immune defenses make people more fragile and vulnerable to infections.
- The other patients and the number of people who travel to a hospital every day. Hospitals are quite crowded places (patients, health staff, relatives, cleaners, etc.); in addition, the large number of sick people facilitates the spread of infectious diseases.
CA-MRSA
CA-MRSA is less common than HA-MRSA, although the number of cases associated with it has increased dramatically (and will likely continue to rise) in recent decades.
The favoring factors are numerous; among the most influential are:
- Attending or living in crowded places, such as schools, prisons and military bases.
- The practice of contact sports, such as rugby, because the skin-to-skin transmission of the pathogen is easier.
- The presence of cuts and grazes on the skin, due, for example, to the use of illegal drugs such as heroin.
- Lack of adequate immune defenses. This can be linked to serious diseases, such as AIDS, systemic lupus erythematosus and cancer, or to organ transplantation.
- Failure to periodically clean very busy environments, with consequent contamination of all surfaces and all objects present. In this regard, it should be remembered that MRSA is a remarkably resistant bacterium.
- Poor personal hygiene. This explains why MRSA is common among the homeless.
- Indiscriminate use of antibiotics, which favors the spread of resistant bacterial strains.
Symptoms and Complications
MRSA can manifest itself with different symptoms and signs, depending on whether the responsible bacterium has infected the skin or has penetrated deeper into the blood and other internal organs of the body.
LOCALIZED MRSA AT SKIN LEVEL
When MRSA is expressed in the skin it can cause boils, abscesses and infectious cellulite phenomena.
Boils and abscesses. A boil is a pus-filled skin protuberance due to a "superficial inflammation of the hair follicles; an abscess, on the other hand, is a collection of pus, bacteria, plasma and cellular debris, which can also form in locations other than the skin.
Infectious cellulite. Infectious cellulitis is an acute and severe inflammation of the dermis and subcutaneous layers (NB: the dermis is the intermediate layer of the skin, located under the epidermis and above the hypodermis). Its onset makes the skin red, warm, soft to the touch, painful and swollen.
According to some estimates, 75% of the forms of CA-MRSA are localized on the skin.
INVASIVE MRSA

Figure: A boil. From the site: prn.org
When the MRSA bacterium manages to pass through the skin (which acts as a protective barrier), and to reach the blood or internal tissues of the body, it can cause unpleasant and sometimes very serious consequences.
In moderate cases, invasive MRSA (as MRSA extended to the blood and internal tissues of the body is called) causes:
- Fever at 38 ° C
- Chills
- Sense of general malaise
- Confusion
- Dizziness
- Muscle aches
- Sense of pain, swelling and numbness in the affected body parts
In severe cases, invasive MRSA can result in:
- Septicemia. It is the medical term used to indicate the persistent presence of bacteria in the blood; this condition is different from bacteremia, with which instead a transient presence of bacteria in the blood is identified.
Severe septicemia can escalate into so-called septic shock, the main sign of which is a marked drop in blood pressure (severe hypotension). - Urinary tract infections (i.e. ureters, bladder and urethra).
- Endocarditis. It is an inflammatory process affecting the membranes that line the internal cavities of the heart and the four heart valves.
- Pneumonia. It is inflammation of the lungs.
- Septic arthritis. It is the inflammation of the joints caused by bacteria.
- Osteomyelitis. It is an infectious process that affects the bones.
- Bunions.
Can MRSA abscesses and infectious cellulitis cause the same symptoms as invasive MRSA?
The answer to this question is: "Yes, when there is a worsening of the conditions and the bacteria reach the blood." chapter dedicated to prevention).
Diagnosis
To find out if there is a "bacterial infection from Staphylococcus aureus, a culture should be performed on a sample of blood (blood culture), urine (urine culture), cells (cell culture), or sputum. Conceptually, they are all very similar procedures: once the chosen biological sample (for example, blood) has been taken, it is inoculated in different culture media, each of which is suitable for the growth of a specific bacterium. If in the soil suitable for the growth of Staphylococcus aureus its reproduction is observed, it means that the bacterial infection in progress is caused precisely by the Staphylococcus aureus.
NEXT STEP: ANTIBIOGRAM
The next step to the "culture test is the" antibiogram, that is the sensitivity test of a microorganism (in this specific case, the Staphylococcus aureus) to one or more antibiotics. This investigation is to find out if it is Staphylococcus aureus found in the patient:
- It is resistant or not to penicillins and cephalosporins (so if it is a strain of MRSA).
- It is sensitive to some particular antibiotic. The antibiotic or antibiotics that have proved effective will then be used during the course of therapy.
Treatment
Therapy for infections with Staphylococcus aureus Methicillin resistant depends on at least three different factors, namely:
- The site of infection, if confined to the skin or extended to blood and some internal body tissue.
- The antibiotic to which the particular strain of MRSA responsible has been shown to be susceptible.
- The severity of the symptoms in place.
WHAT TO DO WHEN MRSA IS ON SKIN?
For boils and abscesses, the most suitable treatment is usually incision of the affected area, followed by drainage of pus. Both of these operations are performed, after local anesthesia, with a sterile needle or scalpel.
For infectious cellulite, on the other hand, the treatment consists in the oral or intravenous administration of one of the antibiotics that are effective in the antibiogram. The duration of treatment, in these cases, is variable and can last from a minimum of 5 days. to a maximum of 14 days.
WHAT TO DO WHEN MRSA IS INVASIVE?
In case of invasive MRSA, hospitalization and a combination of several antibiotics are required (one antibiotic alone, in fact, may not be sufficient). The administration of these drugs is by injection and has a variable duration in relation to the infected organ. (it can be up to six weeks).
What does hospitalization involve?
Patients with MRSA are admitted to the isolation ward in order to safeguard other patients and prevent the spread of the infection. They can receive visits from relatives and friends; these, however, must protect themselves with a gown, mask and gloves, and avoid contact with their loved one.
DECOLONIZATION
Decolonization is the process of eliminating the bacteria present on a colonized individual.
List of the main antibiotics that can be used in case of MRSA:
- Linezolid
- Trimethoprim
- Clindamycin
- Doxycycline
- Minocycline
- Teicoplanin
- Vancomycin
- Daptomycin
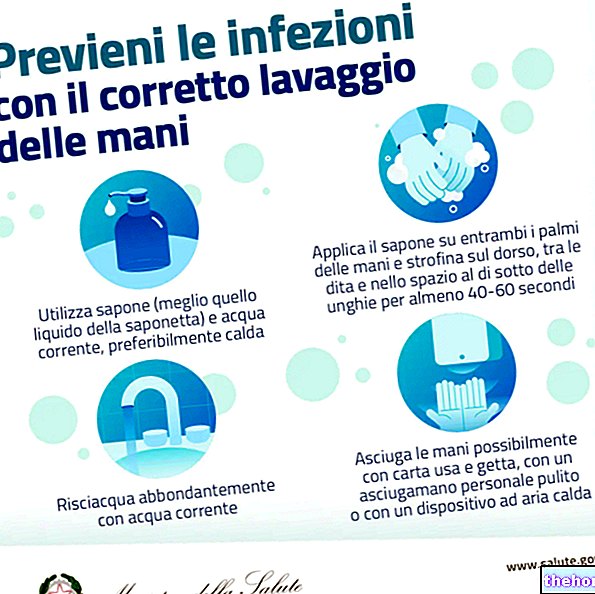
It is achieved by carefully washing the skin (especially the hands), with detergents (soaps and shampoos), disinfectants and alcohol-based preparations.
For good results, it is sufficient to perform the entire procedure once a day for 5 consecutive days.
Prevention
To prevent HA-MRSA, it is good that all patients, health care staff and those who visit sick relatives adopt certain hygiene measures.
Patients should take care to wash their hands after each use of the bathroom and at each meal; in addition, they must ensure that the room and toilet are always properly clean.
The healthcare staff (doctors, nurses and laboratory technicians) must use the indicated clothing (i.e. gown, gloves and, in the case of patients with infectious diseases, mask) and must wash their hands with disinfectant soaps after each contact with patients (albeit minimal).
To prevent CA-MRSA, on the other hand, it is a good idea to:
- Wash your hands several times a day and shower regularly.
- Keep fingernails short and clean. In fact, different types of bacteria can lurk in the nails and, with a long nail, it is easier to scratch or scratch someone else.
- Do not share products that are used directly in contact with the skin, such as soaps, deodorant sticks, etc.
- Don't share the towel.
- Do not share razors, nail files, toothbrushes, hairbrushes and combs.
How to prevent a worsening of MRSA in the skin?
It is a good idea to bandage the affected anatomical area with sterile gauze, at least until you have been examined by the doctor.
Also, if you have touched the MRSA-infected area, you should wash your hands and avoid recycling the used gauze, which should instead be thrown into special waste containers.