Introduction
For a long time, enterococci have been labeled as streptococcal microorganisms belonging - due to their peculiar antigenic characteristics - to the Lancefield group D.

The decision to devise a new genus of bacteria was made following some considerations:
- Enterococci have numerous differences from other streptococci (eg. S. pneumoniae, S. pyogenes, S. agalactiae, etc.)
- They are bacteria that are particularly resistant to the environment
- They also grow on soils with a concentration of NaCl equal to 6.5% and in the presence of bile salts at 40%
- They replicate at a pH ranging from 4.5 to 10.0
- They withstand temperatures ranging from 10 ° C to 45 ° C
- They are able to survive for 30 minutes at a temperature of 60 ° C
- They develop a high resistance to antibiotics and antibacterials
- Enterococci are less virulent than staphylococci and streptococci
Microbiological description
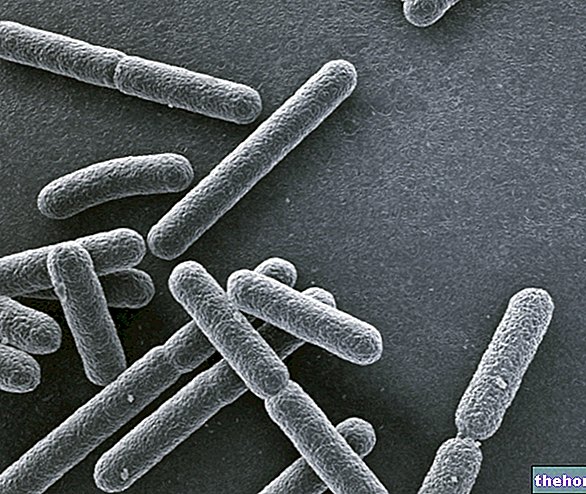
Enterococci are gram positive, catalase negative bacteria with a rounded or oval shape, often arranged in chains. Furthermore, enterococci are generally immobile, aerobic / facultative anaerobic microorganisms having a lactic fermentative metabolism. These cocci, while excellently resisting external environmental conditions, are not spore-forming.
Enterococci are rarely beta-haemolytic; in fact, they often do not generate any hemolysis in blood agar medium. Enterococci are widespread in nature and are often found in the fecal material of vertebrate animals (including humans).
Some enterococci habitually populate the human intestine: among these, we recall E. faecalis (90-95%) and E. faecium, isolated in 90-95% and 5-10% of human fecal specimens, respectively. In addition to these species of enterococci, there are about ten other species, almost impossible to find in the human organism.
Occasionally, these commensal enterococci can cause damage, leading to endocarditis, mastoiditis, abscess and urinary tract infections.
In general, enterococci are practically ubiquitous in the environment. The wide spread of these bacteria may probably depend on their excellent ability to survive and adapt to different temperatures, pH, oxygenation and metal ion concentrations than other cocci.
When enterococci are found in water, we are faced with an evident sign of fecal pollution or a reduced efficiency of the water purification system. Fortunately, at the present time it is observed that the presence of enterococci in water intended for consumption is very rarely reported.
Enterococci and infections
Although they tend to develop a "balanced coexistence with the" host by habitually populating the intestine, enterococci can become pathogenic and cause damage. It must be emphasized, however, that enterococci are decidedly less virulent when compared to streptococci and staphylococci.
The main problem of enterococci is the extraordinary ability to develop resistance to antibiotics (the topic will be further explored later).
Pathologies mediated by enterococci include:
- bacteremia
- bacterial endocarditis
- diverticulitis
- abdominal infections
- urinary tract infections (the most common diseases)
- meningitis (a rather rare pathological condition)
From recent studies it seems that enterococci contribute, in some way, to the onset of chronic bacterial prostatitis.
Furthermore, enterococci appear to demonstrate some ability to adhere to renal epithelial cells and heart valves, developing enterococcal pyelonephritis and endocarditis.
Although the modest virulence of enterococci is ascertained compared to staphylococci and streptococci, the infections sustained by them are not easy to resolve, let alone without complications. In fact, it seems that enterococcal septicemia is burdened by a high mortality, with an "average incidence estimated at around 30-40%.
Mode of transmission
We have analyzed that the major reservoir of enterococci is constituted by the intestinal tract of humans and other vertebrates; more rarely, bacteria also populate the oropharynx, vagina, skin and perianal area.
But how are enterococci transmitted?
It is believed that most of the infections carried by these bacteria are of nocosomal origin, therefore acquired within health and hospital structures. Probably, a similar infection has its roots on an endogenous basis: they are the same enterococci that populate the digestive system. triggering the infection. It seems that the gastrointestinal tract and the hands of nurses, doctors and all health personnel are often contaminated with enterococci. Transmission can also occur through the use of infected instruments.
- Risk factors: many enterococcal infections are acquired in the hospital setting because they are probably favored by the co-presence of other diseases, by the bladder catheter, by neutropenia and by prolonged hospitalization.
Antibiotic resistance
While enterococci cause damage to humans only sporadically, on the other hand the infection they carry is particularly difficult to eradicate. In fact, many enterococci show a high level of intrinsic resistance to penicillins, cephalosporins, aminoglycosides and carbapenems. But that's not all: in the last two years, another strain of enterococci has been isolated that can also develop resistance against vancomycin. These bacteria are known by the acronym "VRE" (vancomycin-resistant Enterococcus) precisely to underline the resistance of these bacteria to vancomycin. VRE enterococci appear to be involved in the emergence of so-called nosocomial infections in hospitalized patients, especially in the United States. Infections sustained by E. faecium can be eradicated with quinupristin / dalfopristin: 70% of patients undergoing this therapy respond positively. Rifampicin and Tigecycline can also be used to ward off pathogenic enterococcus.