The consequences of fulminant hepatitis are often dramatic; the patient, in fact, develops hepatic encephalopathy, coagulation defects, major electrolyte imbalances, renal failure, hypoglycemia and cardio-respiratory problems.
Fulminant hepatitis requires supportive therapy and treatment aimed at restoring liver function.
in charge of:
- The production of essential proteins and hormones;
- The production of clotting factors (essential to stop blood loss);
- The regulation of cholesterol levels in the blood;
- The "cleaning" of the blood from toxins and infectious agents;
- To supply the body with energy when it is in deficit.
A very high dose of paracetamol and its inappropriate use for long periods of time can cause fulminant hepatitis.
The abuse of paracetamol is at the origin of most cases of fulminant hepatitis.
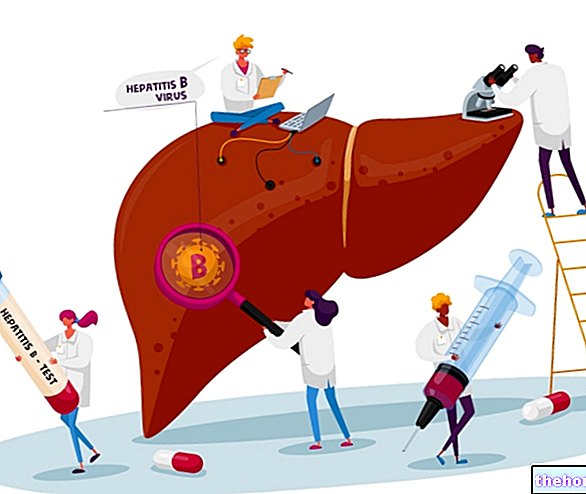
The hepatitis C virus remains out of the list of hepatitis viruses, as experts have not yet clarified whether or not it is capable of causing fulminant liver failure.
It should be noted that fulminant hepatitis sometimes occurs for no identifiable reason.
Pathophysiology of Fulminant Hepatitis
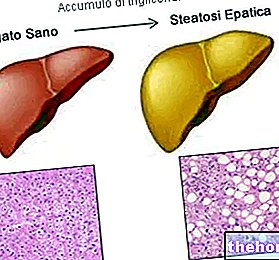
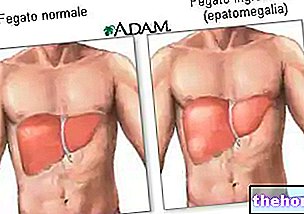
Fulminant hepatitis is characterized by a massive and sudden necrosis of the hepatic parenchyma, and by a decrease in the size of the liver.
All this inevitably leads to a sudden impairment of liver function.
What is a parenchyma?
The parenchyma is the functional component of an organ; in other words, it is that tissue or set of tissues that collaborate with each other to put into practice the function of the organ they are part of. The parenchyma is the set of most important tissues of an organ.
Who Affects Fulminating Hepatitis?
Fulminant hepatitis can affect both individuals with pre-existing liver problems and healthy people who have never suffered from liver problems.
If exposed to one of the potential causes, therefore, anyone can develop fulminant hepatitis.
Epidemiology
The main cause of fulminant hepatitis is the abuse of paracetamol (42% of cases) followed by hepatitis viruses, drugs considered at risk other than paracetamol and mushroom poisoning.
According to some estimates, in the developed countries of the world, fulminant hepatitis would have an annual incidence equal to one case per million people.
liver, bleeding defects (coagulopathy) electrolyte imbalances (hyponatremia, hypokalemia, hypokalaemia and metabolic alkalosis) and hypoglycemia; moreover, very often, it also causes renal failure, systemic inflammatory syndrome (SIRS) and cardio-respiratory problems (hyperdynamic circulation).
The combined renal insufficiency with the hepatic one observed in the presence of fulminant hepatitis constitutes a very serious condition, of absolute danger to life, which takes the name of hepatorenal syndrome.
Hepatic Encephalopathy and Fulminant Hepatitis
Hepatic encephalopathy is a consequence of the inability of the liver (which is in a state of profound suffering) to carry out the cleansing of the blood: a blood polluted by toxic substances and waste, in fact, is a source of damage to the organs and tissues supplied , the brain above all.
Coagulation Defects and Fulminant Hepatitis
Coagulation defects, on the other hand, are a consequence of the liver's inability to produce the so-called coagulation factors: without these factors, the coagulation process is inefficient and, when called into question, does not respond to the needs of the organism.
How does Fulminating Hepatitis manifest itself?
At its onset, fulminant hepatitis manifests with symptoms such as general malaise, fatigue, nausea, and a feeling of discomfort and pain in the stomach.
After a short time, therefore, the condition in question causes jaundice, confusion, drowsiness, personality disorders, irritability, anxiety, disorientation, apathy, amnesia, cognitive deficits, paranoia, easy bleeding and bruising, and ascites.
Fulminant hepatitis evolves quite rapidly; in general, the symptoms reported above can be observed within a few days / a few weeks.
Complications
Many complications are associated with fulminant hepatitis:
- Hepatic encephalopathy causes increased intracranial pressure, papilledema and conditions such as hepatic coma, cerebral edema and cerebral hernia which, even if treated in an adequate and timely manner, are highly fatal.
- Coagulation defects cause thrombocytopenia and increase the risk of brain bleeding.
- Hepatorenal syndrome (association between liver failure and renal failure) is responsible for hypervolemia and damage to other organs of the abdomen; it also contributes to coma.
- Systemic inflammatory syndrome can lead to sepsis.
- Cardio-respiratory problems can lead to tissue hypoxia, hypotension, pleural effusion, pulmonary edema and atelectasis.
When to see a doctor?
"Fulminant hepatitis represents a" medical emergency; therefore, it requires immediate medical attention.
and physical examination;Anamnesis
Anamnesis is the collection of all data relating to the patient, such as age, general health, lifestyle, family history, drugs taken, etc., which can be very useful in establishing the probable reasons for the present condition.
The history of a patient with fulminant hepatitis allows to bring to light situations such as an abuse of paracetamol, the consumption of drugs or herbal products considered at risk, a mushroom poisoning, the presence of Wilson's disease, etc.
Physical examination
The physical examination is the set of diagnostic maneuvers, performed by the doctor, to verify the presence or absence, in the patient, of signs indicative of an abnormal condition.
In a person with suspected fulminant hepatitis, the physical examination consists in palpation of the anatomical area in which the liver is located, in the observation of the color of the skin and ocular sclerae (for jaundice) and, finally, in an accurate evaluation mental status (confusion reflects early stage hepatic encephalopathy).
Liver Health Assessment Test
Liver tests useful for diagnosing fulminant hepatitis are:
- Blood and urine tests that allow to establish liver function (eg: measurement of transaminases; quantification of bilirubin; albumin levels; alkaline phosphatase test, etc.);
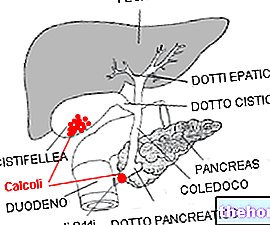
- The diagnostic imaging tests performed at the abdominal level (ultrasound, CT and MRI), thanks to which it is possible to establish liver damage and identify causes such as Budd-Chiari syndrome and liver tumors.
Measurement of prothrombin time and INR
The measurement of prothrombin time and the "INR" is a blood test that quantifies the time required for the quantification of blood clots; in other words, it expresses the speed with which the coagulation process takes place.
In people with fulminant hepatitis, the measurement of the prothrombin time and the INR shows that coagulation takes longer than normal; this anomaly is a consequence of the inability of the liver to produce clotting factors (coagulopathy).
of a hospital is able to guarantee eToday, thanks to medical advances, the treatment options for fulminant hepatitis are more and more effective than they used to be.
Supportive Therapy for Fulminant Hepatitis
Supportive therapy for fulminant hepatitis serves to control the symptoms and complications of the condition; it is essential to avoid worsening and must continue until liver function is restored.
Supportive care for fulminant hepatitis includes:
- Administration of lactulose to control hepatic encephalopathy and prevent / treat cerebral edema;
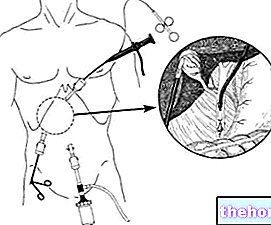
- Nasogastric intubation, if the patient is in a coma;
- Pulmonary artery catheterization and administration of epinephrine, norepinephrine or dopamine to cope with cardiovascular problems;
- The administration of mannitol to reduce the elevated intracranial pressure;
- The use of fresh frozen plasma to counteract coagulation defects; if this remedy is ineffective, the alternative is the injection of recombinant factor VIIa (a coagulation factor)
- Transfusion of platelets, if the patient has thrombocytopenia;
- Renal dialysis, if the patient also suffers from kidney failure.
In addition, during supportive therapy, the patient suffering from fulminant hepatitis is subjected to continuous monitoring of vital functions.
Therapy to restore liver function
Therapy to restore impaired liver function from fulminant hepatitis depends on the underlying cause.
In case of fulminant hepatitis due to the abuse of paracetamol, this therapy involves the administration of a medicine called acetylcysteine; if the causative factor is a mushroom poisoning, it is based on the administration of a specific antidote that cancels the effects of the fungal toxin; if the responsible is a hepatitis virus (eg: HBV), is based on the use of specific antiviral drugs; in all other cases, it corresponds to liver transplantation.
It should be noted that, sometimes, liver transplantation is indispensable even in those circumstances for which canonical therapy for restoring liver functions is "another."
For further information: Liver transplant: what does it consist of?Treatments of the future
Studies are underway to develop new therapies for the restoration of liver functions compromised by a "fulminant hepatitis; among these therapies, the following deserve a mention:
- A medical instrument capable of replacing the functions of the liver, comparable to the renal dialysis used in people with renal insufficiency;
- Hepatocyte transplantation (hepatocytes are the constituent cells of the liver parenchyma);
- Liver transplantation from animals (xenograft).