What is Aortic Dissection?
The term aortic dissection - or aortic dissection, if you prefer - identifies a serious medical condition in which the inner layer (intimate tunic) of the largest artery of the body (the aorta) is affected by a laceration, through which blood enters. and determines the formation of a false lumen.

Commonly, this vascular disease is associated with hypertension, which occurs in more than two thirds of patients. Aortic dissection can be caused by congenital defects and connective tissue disorders, such as Marfan syndrome and Ehlers-Danlos syndrome. Others causes are represented by arteriosclerosis (tissue hardening of the arterial wall) and by degenerative and inflammatory processes affecting the cardiovascular structures. In rare cases, an aortic dissection occurs accidentally during the insertion of a catheter into an artery (for example, during an "aortography or an" angiography) or the performance of a surgical procedure.
Aortic dissection presents with sudden, stabbing pain in the chest and between the shoulder blades. Symptoms may initially mimic those of other diseases, leading to potential delays in diagnosis. However, when an aortic dissection is diagnosed early, the chances of survival are greatly increased. Prompt treatment can therefore help save the patient's life.
Anyone can develop aortic dissection, but the condition is more common in men between 60 and 70 years of age.
Pathogenesis
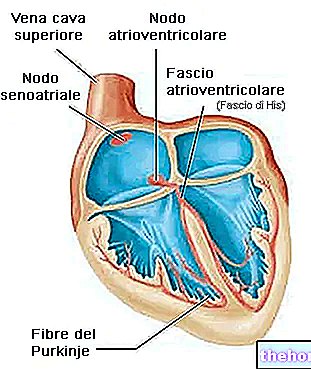
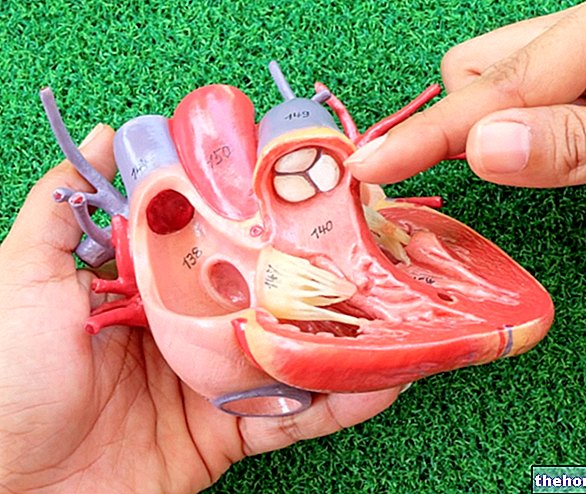
Like all arteries, the walls of the aorta also consist of three superimposed layers: the inner tunic (the innermost), the intermediate tunic and the external or adventitious tunic.
The intima is in direct contact with the blood flowing inside the aorta and is mainly made up of an endothelial lining and the underlying connective layer. The intermediate tunic contains connective and muscular tissue, while the adventitia forms a sheath of Containing connective tissue around the vessel.

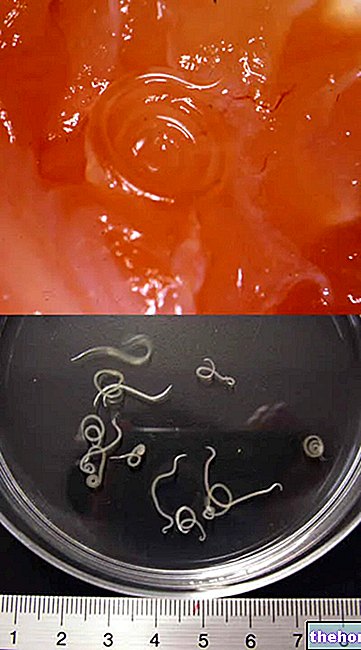
In an aortic dissection, the initial event consists of a tear in the intima of the aorta. Due to the high pressures to which it is subjected, a separation or delamination progressively develops between the layers of the aortic wall (intima and media). This phenomenon allows the penetration of blood under pressure into the intermediate layer and the creation of a false lumen.
The aortic dissection can extend proximally (closer to the heart), distally (away from the heart), or in both directions. If the false lumen extends, it can exert pressure on other branches of the aorta, resulting in the narrowing of the vessels involved and the reduction of blood flow through them.
Predisposing factors
Aortic dissection basically occurs due to the rupture of a weakened area of the aortic wall.
The main risk factors for aortic dissection are:
- Arterial hypertension: makes the vascular tissue particularly susceptible to laceration;
- Arteriosclerosis;
- Inflammations of the aorta;
- Aortic aneurysm;
- Acquired aortic valvulopathies;
- Congenital cardiovascular abnormalities: bicuspid aortic valve (congenital defect of the aortic valve) and aortic coarctation (narrowing of the blood vessel);
- Traumatic injuries: Rarely, aortic dissections can be caused by trauma sustained during a car accident, surgery, or as a complication of cardiac catheterization.
Some diseases are associated with the "weakening" of the aorta and, due to their clinical characteristics, expose the subject to a greater risk of undergoing an aortic dissection:
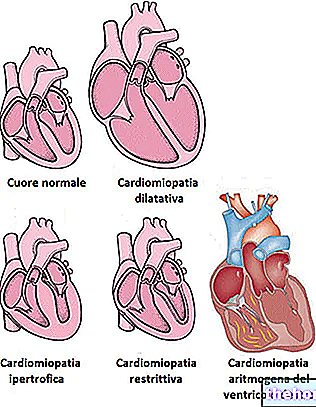
- Marfan syndrome: patients have a congenital predisposition to some alterations of the cardiovascular system. The onset of dissection of the aorta is also a fairly frequent phenomenon, due to the characteristic weakness of the blood vessels resulting from the disease.
- Ehlers-Danlos Syndrome: This group of disorders predominantly affects the connective tissue and is characterized by hyper-elasticity of the skin, laxity of ligaments and fragile blood vessels.
- Turner Syndrome: High blood pressure, heart problems and a number of other conditions can result from this disorder.
Other potential risk factors include:
- Cocaine abuse has been associated with aortic dissection, possibly due to temporary increases in blood pressure and catecholamine spikes;
- Rarely, aortic dissections occur in healthy women during pregnancy;
- Other risk factors are smoking and hypercholesterolemia.
Symptoms
All patients with an aortic dissection experience pain, usually sudden and stabbing, often described as a tear. Commonly, this symptom is felt throughout the chest, but can also be felt in the upper back, between the shoulder blades.
Symptoms of an aortic dissection are:
- Sudden and severe pain in the chest or upper back, often described as a tearing or cutting sensation, radiating to the neck or down the back.
- Loss of consciousness (fainting);
- Dyspnea (shortness of breath);
- Sudden slurred speech, loss of vision, weakness or paralysis of one side of the body
- Sweating;
- Difference in blood pressure in the limbs, on the right and left side of the body.
As the disease progresses, the false lumen can occlude one or more arteries that branch off from the aorta, blocking the flow of blood. The direct consequences vary depending on the blood vessels involved and include:
- Angina, due to the involvement of the coronary arteries;
- Paraplegia, spinal cord ischemia and paraesthesia due to involvement of the spinal arteries;
- Ischemia, due to the involvement of the distal aorta;
- Sudden abdominal pain, with possible intestinal infarction, if the arteries of the mesentery are involved;
- Neurological deficit, if the carotid artery is involved.
When the pressure exerted by the blood exceeds a critical limit, rupture of the external aortic wall (adventitia) can occur. Blood can escape from the aortic dissection and diffuse into the pleural space, mediastinum, or pericardium (between the two layers of membranes surrounding the heart).Pericardial effusion, in particular, can cause cardiac tamponade, a life-threatening condition.
Complications
An aortic dissection can lead to:
- Death, due to severe internal bleeding;
- Organ damage, such as kidney failure;
- Stroke;
- Damage to the aortic valve and aortic insufficiency.
Diagnosis
Early diagnosis can be difficult, as aortic dissection produces a variety of symptoms that sometimes resemble those of other disorders.
The diagnosis can be defined by the following investigations:
- Chest X-ray: This is the first step in identifying some signs of aortic dissection. X-rays show mediastinal enlargement, present in most symptomatic people with ascending aortic dissection. However, the test has low specificity, as many other conditions can lead to the same outcome.
- Computed Tomography (CT) with Contrast: It can quickly and reliably detect aortic dissection, so it is useful in an emergency.
- Electrocardiogram (ECG): it does not have characteristic features, but it can be included in the diagnostic path.
- Magnetic resonance imaging (MRI): MRI is currently the reference test for the detection and evaluation of aortic dissection. An MRI exam produces a three-dimensional reconstruction of the aorta, allowing the physician to determine the location of the intimal tear, the involvement of the vessels and any secondary ruptures.
- Transesophageal echocardiography (TEE): the ultrasound probe is inserted through the esophagus and positioned near the heart and the aorta, allowing a clear "view" of the heart and its structures. TEE makes it possible to detect even very small aortic dissections.
Prognosis and Therapy
An aortic dissection is a medical emergency that requires immediate treatment. Therapy may include surgery or medication, depending on the aortic section involved. Without treatment, about 75% of people die within the first 2 weeks, mostly from complications associated with dissection. With treatment, about 70% of patients with dissection in the first part of the aorta (ascending portion) and about 90% of those who have the disorder without involvement of the ascending aorta have a positive prognosis.
People with an aortic dissection are admitted to an intensive care unit, where their vital signs (pulse, blood pressure, and respiratory rate) are closely monitored. Death can occur a few hours after the onset of the disease. Therefore, as soon as possible, drugs (usually nitroprusside plus a beta-blocker) are given intravenously in order to reduce heart rate and blood pressure, while maintaining a Sufficient blood supply to the brain, heart and kidneys. The reduction in blood pressure helps to limit the extent of the dissection.
Shortly after stabilization with drug therapy, physicians must decide whether to recommend surgery or continue with the administration of drugs. Surgery is often indicated for dissections involving the first few centimeters of the aorta (closest to the heart), except for complications that make the risk associated with the operation too high. For dissections located in regions further away from the heart muscle, doctors may decide to continue drug therapy. However, surgery is always necessary when dissection of the artery causes blood to leak, blocks blood flow to the legs or vital organs, causes severe symptoms to develop, tends to spread, or occurs in a person with the syndrome. of Marfan. During the operation, surgeons remove the affected aorta section, close the false lumen and reconstruct the blood vessel with a synthetic prosthesis. Removal and repair takes approximately 3-6 hours and hospital stay is approximately 7-10 days. In some cases, an endovascular stent may be inserted. This procedure takes 2 to 4 hours and the hospital stay takes approximately 1-3 days.