A hereditary condition, SMA is due to mutations in the SMN1 gene or the SMN2 gene, the purpose of which is to produce a protein that serves to ensure the survival of motor neurons.
There are five different forms of spinal muscular atrophy: type 0, type 1, type 2, type 3 and type 4. The first three types are very serious and cause the patient to die prematurely; type 3 and type 4 are milder variants, which affect the standard of living of the patient, but without causing premature death.
A genetic test on a blood sample is needed to diagnose SMA.
Currently, the therapy of SMA is mainly based on symptomatic treatments, aimed at relieving disorders and controlling complications. A cure is available, based on the principles of gene therapy, but it is a very expensive solution and applicable only to certain patients.
, which manifests itself with atrophy and consequent weakening of the skeletal muscles, and motor difficulties.
SMA is a condition that can cause the death of the patient at a young or very young age: the most serious forms of the disease, in fact, affect the efficiency of the respiratory muscles and are responsible for episodes of respiratory failure or pneumonia with a fatal outcome.
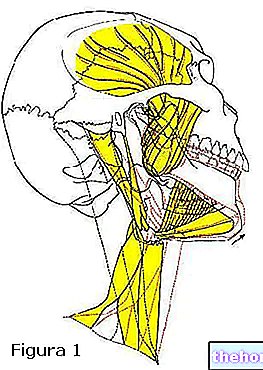
Motor neurons and SMA

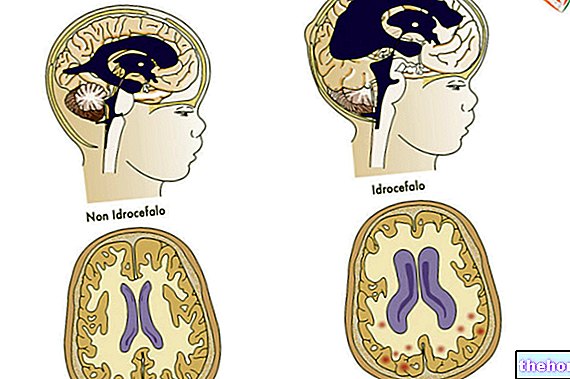
Motor neurons, or motor neurons, are nerve cells that arise in the central nervous system (brain and spinal cord) and which, by means of their extensions (axons), control the activity of muscles and glands.
There are two types of motor neurons: upper motor neurons (or first motor neurons) and lower motor neurons (or second motor neurons).
The upper motor neurons originate in the brain and direct the activity of the lower motor neurons, which arise mainly in the spinal cord and are responsible for directing the activity of the skeletal (or somatic) muscles, of the smooth (or visceral) muscles, of the heart muscle and of the heart.
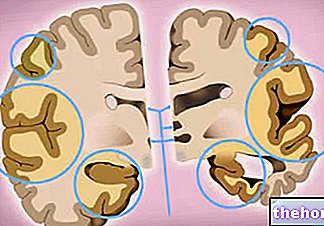
The motor neurons of individuals with SMA degenerate gradually, causing "muscle atrophy from inactivity which, in the most severe cases, results in paralysis, respiratory failure and death.
Epidemiology: how common is Spinal Muscular Atrophy?
SMA has an "annual incidence of 1 case per 10,000 new births.
5 and on which the production of the so-called survival protein of motor neurons (SMN) depends.As the name of the protein produced by SMN1 and SMN2 suggests, the mutation of these genes deprives motor neurons of a biological substance essential for their survival; more precisely, it reduces protein levels: for example, in the presence of mutations in SMN1, the levels of SMN protein drop to 10-20% of normal.
Obviously, the absence of adequate quantities of the SMN protein determines the progressive degeneration of motor neurons.
The loss of motor neurons interrupts the nerve signaling that allows to control the activity of the muscles of the human body; the latter, as a consequence of the fact that they are no longer usable, undergo a gradual process of atrophy and weakening.
Did you know that ...
The SMN2 gene is, for SMA, a disease-modifying gene; in fact, in patients with mutation in SMN1 and who have, for some reason, three or four copies of the SMN2 gene, SMA occurs in a milder form.
Spinal Muscular Atrophy: Types of Mutation
When SMA is due to an "alteration of SMN1, in 95-98% of cases the responsible mutation consists in a deletion of the entire gene, while only in 2-5% in an" anomaly of the normal gene sequence.
Spinal Muscular Atrophy: a Hereditary Disease
In almost all cases (98%), the genetic anomaly responsible for SMA is hereditary, ie it is the parents of the sick individual who transmit it.
2% of non-hereditary cases of SMA are due to a mutation de novo occurred at a very early stage of embryonic development.
SMA and Inheritance model
The inheritance model for spinal muscular atrophy is autosomal recessive, which means that, in order to inherit SMA, it is essential that both parents are healthy carriers of the genetic defect in SMN1 or SMN2 and that both parents pass it on.
In the case of autosomal recessive inherited diseases such as SMA, the probability that both parents with healthy carriers will transmit the genetic defect to the child, thus making him ill, is 25%, i.e. one in every 4 cases.
Types of SMA
Based on the age of onset and the severity of the condition, experts recognize five different forms of spinal muscular atrophy:
- SMA type 0: it is the most severe form of all. It manifests itself even before birth with reduced mobility of the fetus.
Infants usually survive a few weeks after birth, even when they receive respiratory support. - SMA type 1: of the forms that occur during life, it is the most severe and most common (about 50% of cases); it appears at an early age, usually within the sixth month of life.
As a rule, it is the cause of death already in the first years of life; rarely, during adolescence.
Death typically occurs from "respiratory failure or" lung infection. - SMA type 2: it is the form that, by gravity, ranks second; generally, it begins between 7 and 18 months of life.
The life expectancy for those affected is greater than in the previous case: the patients, in fact, manage to reach adulthood. - SMA type 3: less severe than the previous two, this form of SMA typically occurs after 18 months of life (in some cases, it can also occur during childhood or adolescence).
It involves major disabilities, but does not affect life expectancy. - SMA type 4: it is the adult form of the disease as well as the least severe; it usually begins around the third decade of life and has a very slow course.
It is generally not responsible for respiratory problems and is associated with a "normal life expectancy."
The SMN protein levels affect the severity of SMA: the lower the amount of SMN, the greater the severity of the related disease.
The reduction in SMN levels is closely related to the extent of the genetic defect that affected the SMN1 or SMN2 genes: the more extensive this defect is, the more significant is the reduction in the quantity of the SMN protein (this is the case, for example, of a gene deletion).
Furthermore, SMA does not compromise the intellectual functions (the IQ of patients is normal) and spares the organ of sight.
For further information: SMA: all the SymptomsType 0 SMA symptoms
As previously stated, type 0 SMA already occurs in the prenatal age with reduced fetal mobility; at birth, then, the sick child presents evident difficulties in swallowing and breathing.
The disease results in death within a few weeks of birth, even when the patient receives respiratory support.
Type 1 SMA symptoms
Children with SMA type 1 have very weak muscles that do not develop as they should (muscle wasting). This prevents them from doing activities such as lifting their heads, moving their limbs, and assuming a sitting position; moreover, it progressively complicates vital functions, such as sucking milk, swallowing, chewing and breathing.
Typically, type 1 SMA is fatal within the first few years of life; some patients, however, manage to reach the age of adolescence.
Death typically occurs from respiratory failure or a "lung infection due to swallowing difficulties (ingestion pneumonia or pneumonia ab ingestis).
Type 2 SMA symptoms
SMA type 2 classically manifests itself with:
- Softness of the muscles of the arms and legs;
- Tremors in the fingers and hands;
- Difficulty in assuming the sitting position independently (the patient, however, manages to maintain it);
- Difficulty standing and walking
- Deformity and joint problems;
- Difficulty breathing and swallowing food;
- Scoliosis (usually appears later).
Even in this situation, breathing difficulties and swallowing food are the cause of premature death, which generally occurs at the beginning of adulthood.
Type 3 SMA symptoms
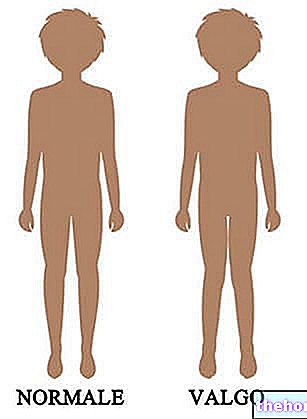
Type 3 SMA causes problems with posture and balance, hand shaking, and difficulty getting up from a sitting position, walking, climbing stairs, and running.
At the beginning, the ailments do not require support for locomotion; subsequently, with the degeneration of a greater number of motor neurons, crutches, walkers and wheelchairs become fundamental.
Although it can happen, it is very rare for patients with type 3 SMA to suffer from breathing problems and swallowing food.
In the presence of this form of SMA, life expectancy is normal, but with all the aforementioned problems.
Type 4 SMA symptoms
With adult onset, SMA type 4 is typically associated with:
- Weakening of muscle tone in the arms and legs;
- Difficulty walking
- Shaking and sudden twitching of the muscles.
Initially, the aforementioned complaints are moderate; in old age, they become more consistent.
Like type 3 SMA, type 4 SMA is not a disease that would affect the patient's life expectancy.
SMA: when to see a doctor?
All parents who know they are a healthy carrier of SMA are strongly advised to consult a pediatrician with expertise in genetic diseases and a geneticist.
If you do not have information of this type, it is good to evaluate month by month the motor development of your child and the functions on which life depends (eg: breathing).
Certainly, the inability to sit or assume the sitting position, the difficulty in feeding, the presence of respiratory deficits and a slender and less toned musculature than that of peers constitute alarm bells.
As for the adult form of SMA, the more or less sudden onset of muscle weakness and difficulty walking is suspected and to be monitored.
Spinal Muscular Atrophy: Complications
The most severe forms of SMA can lead to complications such as:
- Suffocation from food. It is due to the reduced ability to chew and ingest food.
- Respiratory failure. It is a consequence of the inability to control the activity of the respiratory muscles.
- Pneumonia ab ingestis (or inhalation pneumonia). It occurs when foreign material that carries pathogens, such as food, saliva or nasal secretions, enters or accumulates in the lungs.
Pneumonia ab ingestis it is the result of swallowing difficulties. - Paralysis resulting in the use of wheelchairs. It happens when the disease has irremediably compromised the patient's locomotor faculties.
- Malnutrition. It is another consequence of the difficulty in swallowing: the patient, in fact, struggles to feed properly.
It should be noted that, sometimes, tests such as electromyography or muscle biopsy may be used during the diagnosis of SMA.
SMA: Physical Examination and Anamnesis
The physical examination in a patient who may suffer from SMA involves a careful analysis of the symptoms and the search for some typical signs of the disease, such as:
- Weakness and tenderness of the muscles;
- Sudden muscle contractions
- Reduced or absent tendon reflexes.
As regards the medical history, however, this focuses mainly on the patient's family history, in order to establish whether any other family member (parents, siblings, grandparents) complains or complained of a similar symptomatology. obviously, the fact that SMA is a hereditary disease, passed on from parents.
Although they do not allow a definitive diagnosis to be drawn up, physical examination and medical history can provide very useful information, which directs investigations towards carrying out a genetic test.
Clearly, if the patient is a small child, the parents will interact with the doctor during the medical history.
SMA and Genetic Test

The genetic test for the detection of SMA involves the search and study of mutations in the SMN1 / SMN2 genes in a sample of blood cells from the patient.
The presence of genetic alterations obviously means disease.
The analysis of the detected mutations is essential to establish the type of spinal muscular atrophy present and the severity of the condition.
To know the results of the aforementioned genetic test, it is generally necessary to wait from 3 to 4 weeks (the precise waiting times vary according to the genetic center that carries out the test).
SMA: is Prenatal Diagnosis possible?
It is possible to diagnose SMA in the prenatal age.
To do this, you need a genetic test on a sample of fetal cells, obtained through delicate methods such as villocentesis or amniocentesis.
Considering the risk of abortion that characterizes CVS and amniocentesis, doctors pursue prenatal research for any mutations attributable to "spinal muscular atrophy only if there is a family history of SMA behind it or if the unborn child is the child of healthy carriers of the illness.
SMA and Neonatal Screening
It should be noted that in a couple of Italian regions (Lazio and Tuscany) a service is active screening for the early diagnosis of SMA and other serious genetic diseases.
The early diagnosis of these diseases allows the timely planning of the most appropriate symptomatic therapy for the control of symptoms and complications.
Spinal Muscular Atrophy and Planning a Pregnancy
Genetic counseling is recommended for all women seeking pregnancy who:
- They had a child with SMA in a previous pregnancy;
- They have a family history of SMA behind them;
- Are they healthy carriers of the disease or their partner is.
Genetic counseling can help women with these conditions understand what risks a future child is exposed to.
SMA and Differential Diagnosis
There are two pathologies very similar to SMA, which only a "thorough diagnostic investigation recognizes and prevents confusion with" spinal muscular atrophy: these are "spinal muscular atrophy with respiratory distress (SMARD) and" bulbo-spinal muscular atrophy (BSMA or Kennedy's disease); the first is due to a mutation of the IGHMBP2 gene located on chromosome 11, while the second is due to a mutation of the sex chromosome X.
and pharmaceuticals) approved Zolgensma, the gene therapy method for the treatment of spinal muscular atrophy.
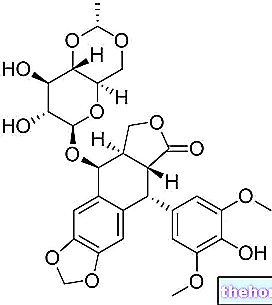
Zolgensma consists of a highly advanced molecular biology technique, which includes the use of a virus-vector capable of inserting a normal copy of the SMN1 / SMN2 gene into the DNA present inside the motor neurons of a patient.
The administration of the aforementioned virus-vector takes place by intravenous injection.
Zolgensma proved effective. However, as anticipated, it has two main limits that prevent its common use:
- It is very expensive. There is talk of millions of euros;
- It is only applicable to SMA patients under 2 years of age.
Spinal Muscular Atrophy: Symptomatic Treatments
Symptomatic therapies for SMA guarantee greater benefits if adopted promptly; this makes early diagnosis of the disease very important.
SMA and Respiratory Support
Proper respiratory support helps SMA sufferers not only breathe, but also reduce the risk of lung infections.
Among the various therapeutic options, there are masks for non-invasive ventilation and more invasive solutions such as orotracheal intubation and tracheostomy; the former are ideal for less severe cases, while the more invasive solutions are essential for patients with serious problems. respiratory.
SMA and Nutrition Support
The most severe forms of spinal muscular atrophy impair the ability to swallow and chew food, exposing the patient to the risk of choking, ingestion pneumonia and malnutrition.
To control these dangerous consequences, it is essential to resort to feeding aids, such as a nasogastric tube or gastrostomy surgery, and to rely on a nutritionist who will plan a diet suited to the patient's needs.
SMA and Physiotherapy
The motor difficulties that characterize the patient with spinal muscular atrophy lead to joint and muscle stiffness from inactivity.
An adequate physiotherapy program allows you to improve, as far as possible, the flexibility of the muscles and make the joints less rigid.
Clearly, this program includes exercises whose execution is within the reach of the patient's abilities.
SMA and Orthopedics
In the presence of scoliosis, typical of severe forms of SMA, it is essential to consult an orthopedist; the latter could indicate the use of an orthopedic corset, if the deformation is mild, or opting for spinal fusion surgery, if the spinal malformation is severe.
Medicines Against SMA
For some years, there have also been specific drugs against SMA.
These medicines deserve a separate treatment compared to symptomatic therapies, although they do not allow to cure the disease, but only to contain it.
The specific drugs against SMA currently available are Spinraza (nusinersen) and Evrysdi (risdiplam): the first acts by correcting the aberrant production of the SMN protein in the process; the second increases the production levels of SMN, also trying to keep them at a quota adequate to the needs of the human organism.
Approved by the FDA in 2017 and 2020 respectively, Spinraza and Evrysdi guarantee results, in some cases even more than satisfactory, however they have an important limitation: they are very expensive.
For further information: Spinraza: How It Works, Risks and Benefits


.jpg)