Edited by Dr. Andrea Gizdulich
Introduction
The increasingly frequent finding of habitual and persistent headaches in patients with anatomical and / or functional problems affecting the stomatognathic system explains the need to include secondary tension headaches among dental pathologies. It should also not be underestimated that the awareness of a link between these two pathologies has also spread among the mass media, influencing public opinion. Understanding the causal relationships existing between the masticatory system and secondary headaches requires a profound knowledge of the pathophysiology of the stomatognathic system, the initial part of the digestive system but also part of the Locomotor System. Equipped with a bone skeleton, joints and a complex and varied musculature possesses a rich innervation and proprioception largely dependent on the second and third branches of the Trigeminal nerve, as well as specific organs such as the teeth, located in the maxillary and mandibular arches. Some peculiarities give this apparatus unique anatomical-functional characteristics in the human body: the mandible, a unique and uneven bone, has two specular joints that bind it to the temporal bones (TMJ), complex in shape and function, owing their ability to ensure rotation and translation movements to the presence of interarticular discs (on which fit the upper heads of the mu external pterygoid scoli).This ensures that the mandible can move in the different planes of space and in practically infinite directions, albeit for modest stretches. The rich masticatory musculature, inserted on both sides of the mandible, is equally obliged to participate in any position or mandibular movement at the same time. Muscle function is essentially carried out by robust levator muscles, by less powerful lowering muscles, because they are assisted by the force of gravity and by other muscles that cause protrusion-retrusion movements. Many cervical muscles cooperate with the chewing muscles, in particular the trapezius and the sternocleidomastoid to which the movement of the head on the neck is entrusted, which consequently determine the position of the upper jaw.

Of all the movements that the mandible can make, the one that causes the maximum possible contact between the two dental arches deserves careful consideration. The position of maximum dental intercuspation, defined as "occlusion" is essential for the chewing function. It is achieved at the end of each masticatory cycle and generally at the beginning of each act of swallowing, ie up to 2000 times approximately in 24 hours. Every single component of the stomatognathic apparatus, muscles, joints, mucous membranes and above all the alveolar-dental ligaments that surround each single root are richly innervated by mechanoreceptors. Consequently, every contact between the dental arches in maximum intercuspation causes a proprioceptive input which influences the tone and the muscular posture, which in terms of number and concentration of receptors, is perhaps unequaled in any other area of the organism. Dental occlusion, conditioned by the number, shape and position of the teeth, is therefore involved in the posture of the head for cervical muscle involvement. Modernly, the occlusion position is considered physiological, which is achieved thanks to an isotonic and balanced contraction of the competent muscles. Whenever this balance cannot be achieved for different reasons, but mostly connected to the situation of the dental arches, there will be an "adapted" occlusion which must be considered pathological.
Pathophysiology of Musculoskeletal Pain
The progress of the clinical knowledge of muscle pain, with its complex syndromic manifestations, in the last twenty years, has been acquired thanks to many scholars, among which the personality of Janet Travell has excelled, whose studies have opened a new fundamental chapter of the diagnosis of one of the most common sufferings.
Pain, defined myofascial because it involves the skeletal muscles and its fasciae and aponeurosis, is preferably established in the muscles with greater postural commitment, both for chronically acting causes (such as the commitment to a forced postural adaptation), and for acute traumatic causes ( such as, for example, the "whiplash"). The pathogenesis of my fascial pain is related to a microtraumatic lesion of the fine muscular structures, sarcolemma and endoplasmic reticulum, which would determine an increase in endocellular free calcium, inducing a stable shortening of the sarcomeres resulting in the establishment of a crisis condition of the muscular energy balance and an inability to re-uptake of Calcium. It has been established that, when the contracture occurs in areas of a muscle where the motor plates are located, there is a condition of dysfunction of certain plates which, by producing acetylcholine in excess with respect to the hydrolysis capacity of cholinesterase, it would lead to a series of vicious circles with increased contracture, capillary spasms, reduced metabolic intake, and also the release of substances with a sensitizing effect on both sensitive and vegetative nerve endings present in the area. The vicious cycle just described would determine the origin of the so-called myofascial trigger points (TrP). A TrP (Fig. 2) is a nodule hyperexcitable placed in a band of tense muscle tissue and therefore available on palpation, which if stimulated gives rise to an intense local painful response, sometimes accompanied by other phenomena such as a local twitch response, referred pain in a well-defined and constant area for each TrP and altered neurovegetative and proprioceptive responses. The most characteristic symptom is referred pain; the pathogenesis of this particular allodynia is not entirely clear; on the other hand, it is known that it always manifests itself in a specific location typical for the TrP that generated it. Since the TrP site is constant in the muscular bodies, due to their interdependence with the locus of the motor plates ("central" TrP) or with the muscle-tendon insertions ("attack" TrP), it was possible to create a map of the areas reference of pain, taking into account that also TrP coming from different muscles can have in common the site of the referred pain.

Aetiopathogenesis and Clinic of Cranio-Mandibular Disorders
The mandibular movement that determines the meeting of the dental arches in occlusion, given its continuous iteration, requires a prompt and direct muscular action. Therefore, the starting position of the mandible, commonly known as the resting position, must be in such conditions as to make this movement instantaneously. The ideal resting position is one in which the musculature is equally in a state of rest, keeping only the basic tone as the only contractile activity. Physiological occlusion can be achieved from the physiological rest position, which totally depends on the efficiency of the dentition. When these conditions do not exist, the chewing and cervical muscles must intervene to create a preventive accommodation of the mandibular rest position in order to make the movement direct and ready. The accommodation takes place through a series of muscular contractions which in reality cancel the situation of muscular rest, instead establishing an overtone of various muscle heads, as can be verified by means of electromyography.
The noxae that can alter the occlusion are many and can act in any age of life; they are linked to disturbances in the development of the maxillary bones, to disturbances of the eruption and subsequent alignment of the teeth, to dental diseases that determine organic damage or even the loss of the sick tooth and finally to causes connected to dental therapies, when they are not able to restore satisfactory morphological and functional conditions of the dental arches. The inevitable consequence of these noxae is the occlusion accommodated in a forced postural position and today rightly considered pathological. The occlusal alteration generates a condition called "Cranio-mandibular Disorder" which can be characterized by different clinical pictures. The clinical picture, in most cases, is devoid of symptoms but instead full of only objective signs that express a condition of precarious balance. When and if this equilibrium were to break, tension headaches and neck pain arise, expression in the head and neck area of the Myofascial Pain Syndrome. Finally, there are clinical pictures complicated by concomitant pathological phenomena affecting the TMJ, forced by the forced dislocation of the mandible, which generate noises and joint impediments of various nature and degree with or without painful manifestations. To better understand the possible myogenic pathogenesis of these headaches, it is useful to consult the map of the reference areas of pain caused by the main TrPs, inspired by the text by Travell and Simons (Fig. 3).

Table 1 - Correlation between headaches and myofascial TrP, according to the criteria of the Classification of Headaches, Cranial Neuralgia and Facial Pain of the International Headache Society.
Diagnostic Procedures
The diagnostic procedures are divided into two distinct phases. The first, entrusted to the criteria of clinical semeiotics, aims to search for the existence of problems affecting the stomatognathic system that justify the diagnostic direction towards the condition of Cranio-mandibular Disorder and towards the possible interdependence between this and the headache, resorting to the "anamnesis", to the examination of the radiograms (generally an orthopantomography of the dental arches is sufficient, accompanied, if necessary, by radiograms of the temporomandibular joints), then to the "objective examination. This in turn requires a "careful inspection of the posture of the head on the neck in anterior-posterior and lateral views and of the shape of the face, with the patient standing; a" careful inspection of the oral cavity in the various components, single teeth and dental arches mucous membranes of the lips and cheeks, tongue, vault of the palate, etc. The movements of the mandible in opening, closing, protrusion and laterality will then be examined; any vibrations and joint noises associated with the movements must be detected and also the possible existence of palpatory joint pain. The complex of specific signs and symptoms collected with these maneuvers is generally sufficient to direct towards a diagnosis of pathological occlusion and associated myofascial pathology. In this case it is necessary to search for the ideal occlusion, which is essential for planning the treatment. For this, the second diagnostic phase, which is computerized instrumental, must be used:
- Surface electromyography;
- Kinesiography (scanning of mandibular movements);
- Sonography to record vibrations and noises produced by the jaw joints in motion;
- T.E.N.S. low frequency;
The diagnostic test begins with the electromyographic recording at rest of the temporal, masseter, digastric and sternocleidomastoid, detected at the mastoid insertion. Other muscle couples, such as the trapezius, can also be recorded.

The test is repeated after the application of T.E.N.S. for about one hour. The comparison between the traces before and after the relaxation induction provides data of great interest. In summary, a generalized decrease in values means the existence of a hypertonic state, with a return to a temporary situation of normality induced by the effect of TENS on the chewing muscles, which in turn allows a relaxed spatial position of the jaw, defined as the "physiological position of rest"
ideal for recording the physiological movement towards the best occlusal contact. It is possible, using the mandibular scan, to observe the movement in the three planes of space, documenting the trajectories of the path traveled. In the case of pathological occlusion, quantitative and qualitative alterations of this path will be observed and it will be possible, by introducing a particular recording material between the teeth, find the position of physiological occlusion represented by an ideal path in a situation of equilibrium of the electromyographic values.
Therapeutic addresses
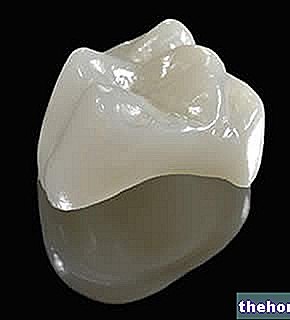
The therapy of pathological occlusion and related symptoms is of the orthopedic type. It consists in the application of an intraoral resin device, preferably applied to the lower arch and constructed according to the findings obtained with the instrumental examination (Fig. 4) .

Table 1