Generality
Atelectasis is the total or partial collapse of a lung, due to the deflation of the pulmonary alveoli.

Figure: Comparison between a healthy lung and a lung affected by atelectasis. From the asbetos.com site
The cause of the alveolar deflation can be a "physical obstruction in the upper airways (for example, an excess of mucus or a foreign body), or an external pressure in the lungs that prevents the lung (s) from taking in air (this is which usually occurs after chest trauma).
Atelectasis can cause respiratory problems, ineffective cough, fever and cyanosis, but it can also be asymptomatic, ie it does not cause any obvious symptoms.
Diagnosis is mainly based on a very common radiological examination, such as a chest X-ray.
Therapy depends on the triggering causes.
What is atelectasis
Atelectasis is the total or partial collapse of a lung, which occurs following a deflation of the pulmonary alveoli.
WHAT ARE THE LUNG ALVEOLUS?
The alveoli are small cavities, located inside the lungs, where gas exchanges between the blood and the atmosphere take place. In them, in fact, the blood is enriched with oxygen, coming from the "inhaled air, and is" freed "of the "carbon dioxide, resulting from" tissue spraying.

Figure: The alveoli are small air chambers, similar to small bags. They are located at the ends of the terminal bronchioles, ie the last branches of the bronchi.
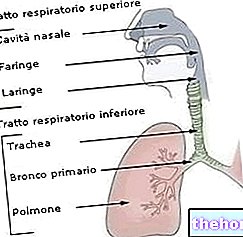
The alveoli reside at the end of each terminal bronchiole; the terminal bronchioles are among the last branches of the airways, which begin with the nasal cavities and continue with the nasopharynx, pharynx, larynx, trachea, primary bronchi, secondary bronchi, tertiary bronchi, bronchioles and, in fact, terminal bronchioles.
The airways are didactically divided into upper airways (from the nasal cavities to the larynx), and lower airways (from the larynx to the alveoli).
Causes
Atelectasis occurs after the deflation of the pulmonary alveoli due to lack of air. But what causes the latter to deflate?
The lack of "air" inside the pulmonary alveoli can be the result of:
- a physical blockage within the upper airways (obstructive block atelectasis);
- an external pressure on the damage of the lung, such that the latter is unable to expand and take in air (non-obstructive block atelectasis or non-obstructive atelectasis).
ATELECTASY FROM OBSTRUCTIVE BLOCK
Physically blocking the passage of air through the upper airways can be:
- A buildup of mucus. Mucus can accumulate when its overproduction is not followed by an "equivalent expulsion by coughing, or when it is not possible to take deep breaths. The accumulation of mucus, moreover, usually occurs both during and after surgical interventions concerning the chest or lung (because the patient cannot cough effectively), in case of cystic fibrosis (which is a very serious genetic disease) and in case of severe asthma attacks.
- A foreign body. Foreign body atelectasis is typical in children when they inadvertently inhale some very small toys or a bite of food (the classic bean or pea).
- The narrowing of the upper respiratory tract due to chronic infections. The infections usually responsible are fungal infections and tuberculosis.
- An upper airway tumor. Tumors cause the growth of an abnormal cell mass within the airways, which blocks the passage of air.
- A blood clot inside the lungs. Formed by a loss of blood, it causes atelectasis when it is not coughed out.
ATELECTASY FROM NON-OBSTRUCTIVE BLOCK
Non-obstructive atelectasis is caused by external compression of the lungs; it can therefore result from:
- A trauma to the chest. The strong blows to the chest, for example following a car accident, cause intense pain, so much so that it is difficult to breathe deeply. The lack of deep breaths progressively reduces the air contained in the alveoli, until they are exhausted.
- A pleural effusion. It is the medical term which identifies an excessive accumulation of fluid (the so-called pleural fluid) inside the pleural cavity. The accumulation is usually due to inadequate disposal.
- Pneumonia. Pneumonia is inflammation of the lungs. Most often caused by viral or bacterial agents, it causes temporary atelectasis.
- A pneumothorax.Pneumothorax is the medical term for the abnormal infiltration of air into the pleural cavity.
- Deep scarring of the lung tissue. Lung scarring can be due to trauma, severe lung disease, or chest surgery. A scarred lung is an inefficient lung at risk of complications.
- A tumor located in the vicinity of the lungs (but not in the upper airways). A tumor that arises near the lungs compresses the latter and blocks the passage of air inside them.
ATELECTASY FROM GENERAL ANESTHESIA
Individuals who, in preparation for surgery, undergo general anesthesia are often the protagonists of episodes of atelectasis. The general anesthesia, in fact, consists in the administration of particular drugs, which can vary the pressure of the gases exchanged inside the alveoli. These variations can sometimes lead to the first emptying of the alveoli and then to the total or partial collapse of the lung (s).
This dangerous mechanism, which usually (if it occurs) occurs at the end of a surgery, is one of the reasons why, after an "operation preceded by general anesthesia, an observation period of at least 24 hours is required.
RISK FACTORS
Atelectasis is more common in some situations and in some individuals.
They are at risk:
- premature babies, because their lungs are immature and lack the right amount of surfactant (N.B: surfactant is a liquid composed of proteins and lipids, essential for good lung health);
- those who, due to different pathological conditions (asthma, cystic fibrosis, etc.), produce a lot of mucus and are unable to breathe or cough effectively;
- people confined to bed and almost total immobility;
- and people returning from surgery on the abdomen or chest;
- people who have undergone general anesthesia a few hours before;
- those who cannot breathe deeply due to chest or abdominal trauma;
- those suffering from some muscular dystrophy;
- people with a spinal cord injury;
- small children (12-36 months), as they more frequently inhale objects or bites of food;
- smokers, because smoking promotes the production of mucus;
- finally, obese people, because the abdominal fat pushes the diaphragm upwards and the diaphragm, thus modified, prevents the lungs from fully expanding.
Symptoms and Complications
Atelectasis can be asymptomatic, ie it does not cause any obvious symptoms. Other times it is characterized by manifest symptoms and signs, which usually consist of: breathing difficulties (dyspnoea), weak but rapid breathing, ineffective cough, low oxygen saturation, high heart rate and mild fever.
In rarer cases, cyanosis and chest pain may also appear.
WHEN TO SEE THE DOCTOR?
When atelectasis is characterized by obvious manifestations, the most characteristic sign that deserves medical attention is difficulty in breathing.
COMPLICATIONS
In an advanced stage, atelectasis can lead to various complications, sometimes even very serious and dangerous, such as:
- Low levels of oxygen in the blood (hypoxemia). An atelectatic lung (ie affected by atelectasis) does not allow the gaseous exchanges that "load" the blood with oxygen, therefore the circulating blood will inevitably be poorly oxygenated
- More or less evident scarring of the lung tissue. The damage that traumatizes the atelectatic lung (s) could be so severe as to leave more or less deep scars. Lung scars represent a serious danger to the patient who is a carrier.
- Pneumonia. Atelectasis pneumonia occurs when there is a buildup of mucus in the collapsed lung. The mucus, in fact, is an ideal place for the proliferation of bacteria and other pathogens.
- State of respiratory failure. Typical of more severe cases or people with severe lung disease, it is the inability to breathe effectively.
Diagnosis
To diagnose atelectasis requires a very simple radiological examination, called a chest x-ray or chest x-ray. This examination shows quite clearly what the lung looks like and which part of it has collapsed (if the collapse was partial); however, very often it does not clarify the triggering causes.
For the latter, more in-depth examinations are needed, such as CT, ultrasound, oximetry or bronchoscopy.
Tracing the causes of atelectasis is extremely important, as it allows the doctor to plan the best and most appropriate treatment for the case.
RADIOGRAPHY OF THE CHEST

Figure: Postero-anterior chest radiograph; red arrows indicate atelectasis of the lower left lobe. Note the underlying elevation of the left half of the diaphragm.
From the site: www.med-ed.virginia.edu
Chest x-ray, or chest x-ray, is a radiological examination that allows the visualization of the main thoracic structures: the heart, lungs, major blood vessels, most of the ribs and a portion of the spine.
The resulting images are obtained from the patient's exposure to a certain dose of ionizing radiation (X-rays); these images, commonly called X-ray plates, are quite clear and sufficiently comprehensive. However, they do not always clarify the exact origin of the atelectasis. .
CT scan
Computed Axial Tomography (CT) is a more sensitive imaging test than chest x-ray, which can show the collapsed lung from multiple angles.
It is particularly suitable for recognizing tumors at the thoracic level.
The CT scan exposes the patient to a non-negligible dose of ionizing radiation.
ULTRASOUND
Ultrasound is a completely bloodless imaging test for the patient. Using ultrasound, lung ultrasound shows what the pleural cavity looks like and whether there is an abnormal accumulation of pleural fluid (pleural effusion).
OXIMETRY
Oximetry is a very simple test, which measures the oxygen saturation in the blood. To do this, it relies on an instrument, called an oximeter, which is applied to a finger or to an earlobe (in both cases, it is a matter of two highly vascularized areas).
BRONCOSCOPY
Bronchoscopy is a diagnostic, and in some cases even therapeutic, procedure aimed at exploring larger airways, such as the larynx, trachea and bronchi. The examination is performed by inserting a tube-probe into the nose or mouth. (called a bronchoscope) very thin, flexible and equipped with a fiber optic camera.
The use of the bronchoscope allows the doctor to identify mucus accumulations, tumors present inside the upper airways and inhaled foreign bodies.
Treatment
The therapy for episodes of atelectasis depends on the triggering causes and is based on the principle that, by "freeing" the airways from the obstruction, the alveoli fill up again with air.
Since mucus occlusions are among the most frequent reasons of atelectatic lung, the attention of this article will focus above all on the so-called thoracic physiotherapy for mucus mobilization, on mucolytic pharmacological treatments (that is, which thin mucous secretions) and on cleaning, by means of surgery, airway.
However, before analyzing the aforementioned treatments one by one, it is good to remember that, in the case of non-severe partial atelectasis, healing can occur even without any particular treatment.
THORACIC PHYSIOTHERAPY
Thoracic physiotherapy, also known as respiratory physiotherapy or respiratory rehabilitation, consists of a series of techniques aimed at: improving deep breathing, allowing adequate expansion of the lungs and, finally, mobilizing the mucus that occludes the upper airways.
Chest physiotherapy is of fundamental importance in case of recovery from chest surgery (for a lung problem but not only) or abdomen, but also in case of cystic fibrosis. The therapist's job is to teach the patient:
- How to cough effectively
- How to beat the chest to mobilize the mucus
- How to use the VestTM system, i.e. the airway clearance system, which serves to mobilize excess mucus.
- Techniques for improving deep breathing. For this purpose, incentive spirometry is also considered effective, which involves the use of a respiratory instrument built specifically to encourage deep breaths.
- Postural drainage techniques. Postural drainage consists of a series of maneuvers and positions aimed at removing mucus from the lungs.
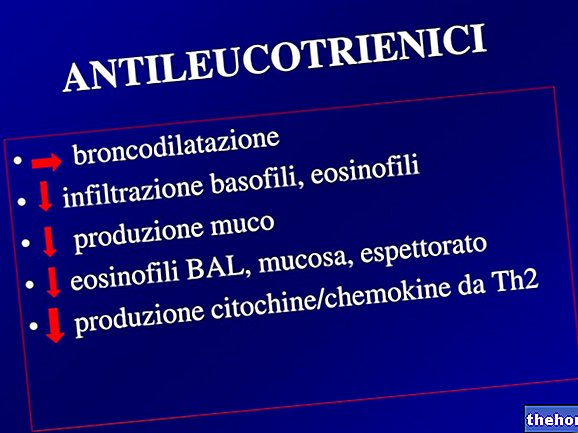
PHARMACOLOGICAL TREATMENTS
Medicines suitable for cases of atelectasis are: inhaled bronchodilators (or inhaled bronchodilators), acetylcysteine-based medicines (such as Fluimucil and Solmucol) and Pulmozyme.
Going into more detail, inhaled bronchodilators "open" the pulmonary airways (bronchi and bronchioles), facilitating breathing and mucus mobilization. Medicines based on acetylcysteine, on the other hand, thin the mucous secretions, thus facilitating their expulsion. Finally, Pulmozyme is used in the case of cystic fibrosis to dissolve the mucus located inside the bronchi. Its mechanism of action is based on the destruction of the DNA of the cells that make up the mucous secretions.
CLEANING OF THE AIRWAYS BY MEANS OF SURGICAL INTERVENTION
When the pulmonary airways are severely obstructed, the doctor may have to resort to surgery, such as tracheo-bronchial aspiration and operative bronchoscopy.
Tracheo-bronchial aspiration, or bronchoaspiration, serves to free the nasopharyngeal tract, trachea and bronchi from mucus, saliva, blood and other abnormal pulmonary secretions. It is a rather invasive, annoying and potentially dangerous procedure for the patient. , because it involves the insertion (nasal or oral) of a flexible and sterile tube, called a tube. The tube, once conducted in the obstructed points, is connected to an aspirator, which sucks up the unwanted material. Bronchoaspiration is carried out only if strictly necessary.
Bronchoscopy has already been discussed previously, during the diagnostic procedures. In fact, the principle by which the upper airways are cleared is not very different from "tracheo-bronchial aspiration, however there is a difference: the bronchoscope is also useful for the removal of tumors and foreign bodies.
Prognosis
The prognosis depends on the severity of the atelectasis and the reasons for its onset.
If the collapse is complete and is due, for example, to cystic fibrosis, the prognosis tends to be negative. Conversely, if the collapse is partial and subsequent to a treatable cause (for example after a "general anesthesia), the prognosis tends to be positive (or at least not negative).
Prevention
To prevent atelectasis, or at least reduce the chances of its occurrence, it is advisable:
- Supervise very young children when they play with small and potentially dangerous objects.
- Avoid giving children under 3 certain foods, such as peanuts, peas and beans, as they are easily inhaled foods.
- Do not smoke, as smoking increases mucous secretion.
- Often change position when in bed, to promote mucus mobilization (N.B: This is particularly suitable advice for individuals at risk of atelectasis).
- Continuously practice respiratory rehabilitation exercises, taught precisely as a countermeasure to atelectasis.